The rate of leukocytes in the blood in children
The number of white blood cells is of great importance for detecting various diseases in a child. Therefore, parents should know how many leukocytes should be normal in children, what is leukocytosis in the blood of a child, and why the number of such cells may decrease.
The role of leukocytes and their types
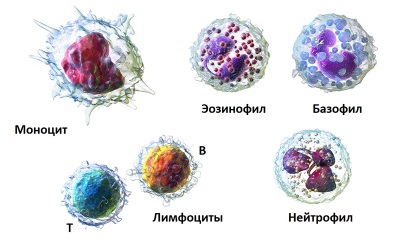
Leukocytes or white bodies is a group of blood cells that protects the child's body from various external influences. Unlike other blood cells, leukocytes are heterogeneous and are represented by different types:
- Neutrophils are the most numerous group of white blood cells with granules, a feature of which is the presence of forms at different stages of maturation (young, young, mature). The main task of such cells is the fight against bacteria, and on the basis of an assessment of the ratio of the forms of neutrophils, one can judge the presence of various pathologies.
- Eosinophils are represented by cells that also have granules. Such white blood cells are designed to protect the children's body from allergens, as well as from parasites and protozoa.
- Basophils are less numerous than other white blood cells with granules. The main task of such cells is the release of biogenic amines into the blood in order to ensure certain immune responses.
- Lymphocytes are a large group of leukocytes without granules, necessary for immune responses. Such cells protect the child from viral infections.
- Monocytes are called a type of white blood cells without granules that can absorb bacteria, dead cells and other substances in order to remove them from the child’s body (they become macrophages).
- Plasma cells are the least numerous group of white blood cells whose task is the formation of antibodies. Such white bodies are normally found only in children.
What affects the number of leukocytes
The number of white blood cells may vary depending on:
- Age The maximum number of leukocytes in the bloodstream is observed in the newborn, and as the baby grows, their number gradually decreases. That is why for the correct interpretation of a blood test it is important to know the age of the child, because, say, the results at 5 months, 2 years or 3 years will differ.
- Physical activity of the child. After a load, for example, an active game or running, the number of leukocytes will increase for a while. Also, their increase can be conditioned by emotional stress.
- Eating Within a few hours after it, the child will be diagnosed with leukocytosis.
- The presence of various diseases. In some pathologies, the number of leukocytes increases (sometimes several times), while in others it decreases.
How to determine the number of leukocytes
Determining the number of white blood cells occurs during the clinical analysis of blood simultaneously with the count of the number of red blood cells, platelets, determining the level of hemoglobin, ESR, hematocrit, and other indicators. Blood for such an analysis is often taken from the finger, but in some cases venous blood is evaluated, and in a newborn baby blood can be drawn from the heel.
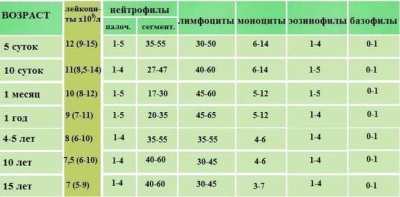
The number of different types of leukocytes is determined separately and displayed as a percentage, which is called a leukocyte formula. Its assessment helps in the diagnosis of specific diseases, because in some diseases there will be an increase in neutrophils, in others there will be more eosinophils, and some diseases are characterized by an increased number of lymphocytes. However, first of all, the doctor will evaluate the total number of leukocytes, so it is on his changes that we will stop.
How to take an analysis
In order for the white blood cell count to correspond to the real picture, it is important to consider the following points:
- A child should not eat at least 8 hours before donating blood, and if it is a baby, then the break from feeding to blood collection should be at least 2 hours.
- Do not allow a child to run before passing the test. It is best to come to the clinic in advance and for 10-15 minutes before taking blood to sit quietly in the hallway.
- Try to reassure the child, so that he does not worry before donating blood and does not cry, because emotional stress affects the results.
- Do not let the temperature drop, so do not go into the office to donate blood immediately after you came to the clinic from the street.
Table by age
The number of white blood cells in normal children of different ages is represented by such indicators:
|
Newborns |
10 to 30 x 109/ l |
|
From the 5th day of life |
9 to 15 x 109/ l |
|
From 10 days of life to 1 month |
8.5 to 14 x 109/ l |
|
In infants from 1 to 12 months |
8 to 12 x 109/ l |
|
In children 1-5 years |
7 to 11 x 109/ l |
|
Aged 5 to 15 years |
6 to 10 x 109/ l |
|
In adolescents older than 15 years |
5 to 9 x 109/ l |
Leukocytes above normal
If a number of leukocytes were identified in the blood test and the indicator exceeds normal, this condition is called leukocytosis. It happens in diseases and when exposed to certain external factors that do not pose a danger to children. Also important for assessing leukocytosis is to determine its severity, since it is directly related to the activity of the pathological process.
In the next video, Dr. Komarovsky will try to answer the question of what leukocyte elevation means in a blood test.
Causes of Leukocytosis
As noted above, a large number of leukocytes can be observed in non-hazardous conditions, for example, after exercise, stress, crying, fright, hot baths, or eating. Pathological leukocytosis in children is diagnosed:
- With bacterial infections, for example, with sore throat or pneumonia.
- After surgery, for example, with appendicitis.
- With a chronic inflammatory process in the body of a child, for example, with arthritis or inflammation of the intestine.
- For viral infections, for example, for hepatitis, ARVI, rubella, HIV infection and others.
- With allergies.
- With fungal infection, as well as parasitic invasions.
- With autoimmune diseases.
- After injury or with extensive burns.
- When cancer pathologies.
- With hemolytic anemia or severe blood loss.
- After removal of the spleen.
- With damage to the bone marrow by various factors.
- After the use of certain drugs, for example, hormonal or immunostimulatory.
Symptoms of leukocytosis
In many children, leukocytosis is manifested by fever, decreased appetite, weakness, dizziness, sweating, fatigue, poor sleep, pain in joints and muscles, weight loss and other symptoms characteristic of infectious diseases, poisoning, cancer, chronic inflammatory diseases and other pathologies, accompanied by high leukocytes.
How to reduce white blood cell count
When a leukocytosis is detected in a blood test, the doctor will refer the child for additional examinations, because such a condition is a sign of an inflammatory process in the children's body. As soon as the cause of high leukocytes is detected, the child will be prescribed the necessary treatment, and when the baby recovers, the level of white blood cells will normalize.
Leukocytes below normal
If the blood test form indicates that there are fewer white blood cells than there should be at this age, this is called leukopenia. This condition is rare in healthy children and often indicates the presence of a disease. The main danger of leukopenia is the weakening of the protective forces of the child’s body, for leukocytes that can fight viruses, parasites, allergens, bacteria and other harmful factors are not enough.
Causes of Leukopenia
A decrease in the number of white blood cells is observed:
- When hypovitaminosis, depletion or starvation.
- With bacterial infections.
- After poisoning.
- Because of taking certain medications, such as cytostatics, antibiotics, anticonvulsants, steroid hormones, and other drugs.
- For viral infections, such as rubella or chicken pox, especially during the recovery period.
- Due to bone marrow damage by radiation, medication, genetic disease, tumor, autoimmune disease and other factors.
- With a decrease in blood pressure.
- For tumors, for example, leukemia.
- In systemic diseases, including lupus erythematosus.
- With anaphylactic shock.
- With hypothyroidism and diabetes.
- With increased activity of the spleen.
Symptoms of leukopenia
There are no characteristic signs of leukopenia, however, this condition threatens the child with the "addition" of an infection, which will manifest itself as fever, tachycardia, weakness, swollen lymph nodes, headaches and other symptoms.
What to do
In case of accidental detection of leukopenia, an additional child should be examined. If the index is reduced slightly and this is due to hypovitaminosis, therapy is limited to the use of vitamin preparations and diet correction. If any serious illness is found, the child is prescribed a suitable treatment. For some time after recovery, the number of leukocytes is restored to the age norm.
Watching the next video, you can learn more about how important leukocytes are in the blood and what is fraught with deviations from the norm.