Thrombocytopenic purpura in children
Hemorrhagic pathologies are specific blood disorders. In children's practice, they occur quite often, differ in a rather heavy course. Quite often in children occurs thrombocytopenic purpura.
Etiology
Currently, there are many hemorrhagic pathologies. For their development lead a variety of reasons. One of these diseases is thrombocytopenic purpura. This pathology tops the list of hemorrhagic diseases in both children and adults. If you focus on statistics, it can be noted that it occurs in 40-70% of patients with various blood pathologies.
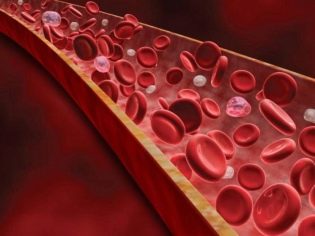
This pathology is characterized by a strong decrease in the peripheral bloodstream of the total number of platelet cells. This is due to the presence of an immune conflict between the blood plates and antigens. It should be noted that the anatomical parameters of the spleen remain normal. Doctors note that more and more cases of this hemorrhagic disease are recorded every year.
Babies suffer from this pathology much more often than boys.
The single cause of the disease is currently not established. For a long time, scientists could not understand the reasons why babies have this blood pathology. Only modern developments and scientific research helped specialists to get some answers to their questions.
The development of thrombocytopenic purpura leads to the influence of various factors. The most common and scientifically sound are:
- Long-term use of certain types of drugs. Scientists have proven that more than 60 different drugs can provoke in a child the appearance of symptoms of this hemorrhagic disease on the skin. Such drugs include quinine, quinidine, sulfonamides, heparin, furosemide, dipyridamole, digoxin, acetylsalicylic acid metabolites, paracetamol, some types of beta-blockers, thiazides, cephalosporins, ampicillin, levamisole and many others. Predicting the development of a hemorrhagic disease in a particular child is an almost impossible task.
- Genetic defects. Many European scientists believe that heredity plays a very important role in the development of the idiopathic version of the disease. Numerous scientific experiments are underway that should prove or disprove this theory. Existing genetic disorders can lead to the development of autoimmune inflammation and the appearance of adverse symptoms of hemorrhagic disease.
- Consequences of infectious pathologies. The toxic effects of the vital products of pathogenic microorganisms on the children's organism leads to the development of various inflammatory immunological reactions. In babies with congenital immunodeficiency states, the risk of thrombocytopenic purpura is increased several times.
- Intrauterine infection. The first signs of hemorrhagic disease are formed in the baby while still in the womb. A woman suffering from thrombocytopenic purpura can pass a series of autoimmune antibodies through the placental blood flow system to the child. This clinical situation leads to the fact that the adverse symptoms of the disease occur in a newborn baby already in the first months of life.
Pathogenesis
For a long time, scientists could not establish what is the mechanism of the development of thrombocytopenic purpura in children. For many decades, various theories persisted that explained the pathogenesis of this hemorrhagic disease. Recently, in connection with the advent of new laboratory apparatus and the improvement of diagnostic methods, new knowledge about the mechanism of the occurrence of thrombocytopenic purpura in children has appeared.
During the pathological process, a large number of specific protein molecules appear in the child’s body. They are called anti-platelet antibodies. These substances begin to interact with the specific antigenic components of the cell membranes of the blood platelets (platelets).
Normally, these blood cells perform a number of very important physiological functions. They are necessary for ensuring normal viscosity, and also for a blood-groove.
The results of recent scientific studies confirm that the structure of platelets in a given hemorrhagic disease undergoes a series of changes. A pronounced granular apparatus appears in them, and the level of alpha serotonin significantly increases. The change in the total number of platelets affects the appearance of persistent changes that begin to occur in the vascular wall. In response to this condition, the amount of platelet growth factor increases.
All these disorders lead to the death of endotheliocytes - the cells lining the inside of the blood vessels and giving them the specific "smoothness" necessary for uninterrupted blood flow. As a result of such pathological abnormalities, the first signs of a hemorrhagic syndrome begin to appear in the child, which significantly worsens his well-being.
After bacterial or viral infections, antiplatelet antibodies usually appear after ½ -1 month. According to their affiliation, they belong to the class of immunoglobulins G. This also explains the persistent persistence of antibodies in the blood in the future. In some cases, they can persist in the child throughout life. The death of "spent" immune complexes occurs in the spleen.
The latest results of scientific studies have made it possible to clarify why a child suffering from autoimmune thrombocytopenic purpura has symptoms of increased bleeding for a long time. This is largely due to a decrease in serotonin levels. Normally, this substance is involved in the formation of a blood clot.
Kinds
Doctors distinguish several clinical forms of this hemorrhagic state.
These include:
- immune thrombocytopenia;
- idiopathic.
Doctors also use another classification, which allows you to separate different variants of thrombocytopenic purpura into different immune forms. These include:
- Isoimmune. Most often after blood transfusions. It can be innate - when the mother and the future baby have an immune conflict on platelet antigens. May have a transient character. This clinical form is often constantly recurrent.
- Autoimmune. Occurs due to the formation in the body of a large number of platelet antibodies to its own blood plates.
- Heteroimmune. The development of this immune variant of the disease often leads to taking certain groups of drugs. An important role in this is played by the presence of individual hypersensitivity and immunity of certain chemicals in a sick baby. This contributes to the development of a specific symptom - purple skin lesions, which are the result of multiple hemorrhages.
- Transimmune. This immune form of the disease develops, as a rule, as a result of the antigenic conflict that has arisen and the accumulation of anti-platelet antibodies in a pregnant woman.They easily penetrate into the fetus through the system of placental blood flow, leading to the development of hemorrhagic syndrome.
Symptoms
The severity of adverse clinical signs of the disease depends largely on how critical the reduction of platelets in peripheral blood. Symptoms increase when the level of the blood platelets drops to 100,000 / μl. Reduction to 50,000 / μl leads to the appearance of pronounced symptoms of hemorrhagic syndrome.
This pathological condition is the most specific clinical sign of thrombocytopenic purpura. It is characterized by the appearance of numerous and diverse hemorrhages that occur in a wide variety of anatomical zones.
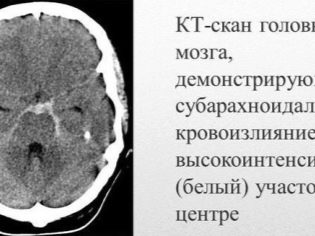
Quite often, a sick child has nasal and gum bleeding, hemorrhages in the brain and internal organs are most dangerous. This leads to disability of the sick baby.
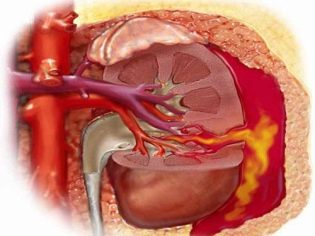
Bleeding in the kidneys or urinary tract is manifested in a child by the presence of blood in the urine. With heavy bleeding, hematuria can occur - the appearance of a large number of red blood cells in the urinary sediment. Bleeding in the gastrointestinal tract (especially in the distal intestine) leads to the fact that the child appears black stools (melena). These clinical signs are very unfavorable and require the obligatory treatment of the advice of a doctor.
Hemorrhagic syndrome in thrombocytopenic purpura has several features. It is characterized by the asymmetry of the resulting deviations, as well as by the complete spontaneity of their appearance. The severity of symptoms, as a rule, does not correspond to the intensity of the impact.
In some cases, the adverse symptoms manifest in a child even with a single dose of the drug or after transferring a normal infection. Quite often, thrombocytopenic purpura occurs in an acute form.
Hemorrhages can be multiple and occur simultaneously (in a variety of internal organs). There are quite unfavorable localization of internal bleeding. These include the kidneys, adrenal glands, head and spinal cord, heart, liver. Hemorrhages in these organs lead to a pronounced impairment of vital functions.
Thrombocytopenic purpura has certain features. During palpation of internal organs, it can be noted that there is no enlargement of the spleen and liver. Lymph nodes also remain normal in size. These clinical signs significantly distinguish this pathology from many other hemorrhagic diseases. Quite often, the syndrome of increased bleeding remains only one manifestation of this disease.
How does it appear in newborns?
The first symptoms in babies who have auto-thrombocyte antibodies in their blood appear in the first months of life. In infants, hemorrhagic syndrome can be expressed in different ways. The appearance of negative symptoms is affected by the initial state of the baby, as well as the presence of severe associated pathologies.
There is thrombocytopenic purpura in children with the appearance of hemorrhages in the skin, mucous membranes, as well as in the internal organs.
Usually, the first symptoms that parents find in a sick child are large bruises that suddenly appear on the skin. As a rule, there are no previous damages or impacts before the appearance of such elements on the skin. The development of hemorrhages in the cavity of large joints is very dangerous, as it can lead to gait disturbance and the appearance of pain when making active movements.
Diagnostics
You can suspect the disease when a child has various hemorrhages. Normally, there are no such manifestations in babies.The appearance of bruises on the skin without regard to injury or shock should also motivate parents to contact the pediatrician with the baby for consultation. A more accurate diagnosis can put the children's hematologist.
For the diagnosis requires several laboratory tests. These studies help to establish the pathological variant of bleeding, as well as determine the severity of the physiological disorders present in the child.
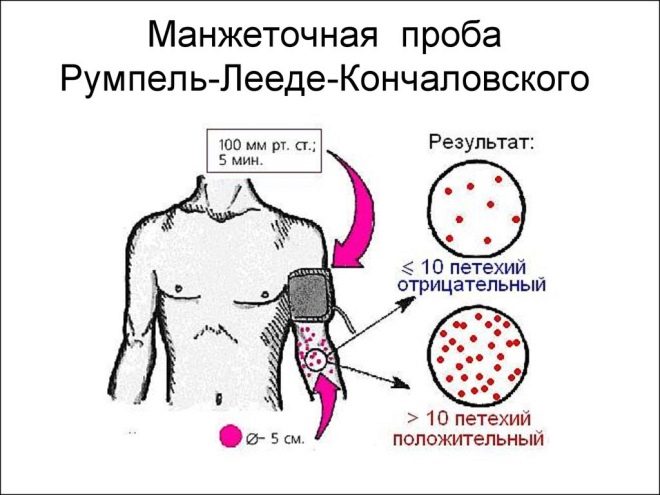
A pinch test and a cuff test are performed to detect excessive bleeding. The study with the help of a cuff of a children's blood pressure monitor for blood pressure measurement is mandatory for the diagnosis of thrombocytopenic purpura.
The basic research that is carried out for all babies, without exception, is a complete blood count. This hemorrhagic disease is characterized by a sharp decrease in the number of platelets. After past viral infections, persistent lymphocytosis may be present in the blood for a long time. Spinal puncture with thrombocytopenic purpura is only an auxiliary one. The result of myelogram with this disease will show that the number of platelets is normal.
In order to establish the existing functional impairment, a coagulogram analysis is performed. It helps determine the amount of fibrinogen, prothrombin time and other important criteria for assessing intravascular thrombosis. The result is evaluated by the attending physician.
In some situations, expansion of the complex of diagnostic measures is required. The purpose of additional research is carried out according to strict medical indications.
Treatment
The appearance of signs of pronounced hemorrhagic syndrome in a baby is a reason for hospitalization. Correction of hematological disorders is carried out in hospital conditions, all processes are controlled by doctors. During exacerbation of the disease bed rest is necessary. As you feel better, your baby can return to his usual way of life. Active sports for these children are usually limited.
One of the important components of treatment is diet.
A sick baby should eat 5-6 times a day, in small portions. Very good, if the food is pre-crushed. It is recommended to cook dishes in a gentle way, roasting in oil should be excluded. The basis of the children's diet should be a variety of protein products.
The main drugs prescribed by doctors to compensate for hemorrhagic syndrome are glucocorticosteroids. They have a complex effect that includes a desensitizing, anti-inflammatory, immunosuppressive and anti-allergic effect. The main drug that is prescribed during this period is prednisone. The dosage of the hormone is determined individually, taking into account the age and weight of the baby.
When you receive prednisone in the blood of a sick child, the number of platelets gradually increases. Acceptance of hormones helps to reduce the number of circulating anti-platelet antibodies, as well as reduce the formation of immune complexes that cause the appearance of adverse symptoms.
About what is thrombocytopenic purpura, see the following video.