Do I need to express colostrum after childbirth and how to do it?
Every woman who has become a mother wants to establish a lactation as soon as possible and provide her baby with useful and necessary breast milk in sufficient quantity. However, as is known, this number does not appear immediately after birth, and the woman is faced with the question: should it be necessary to express the colostrum, so that full-fledged breast milk should appear quickly? We will try to give an answer to it in this article.
What it is?
Colostrum is the secret of the breast. His education begins during pregnancy. This is the first stage of lactogenesis, and it is the longest. In some expectant mothers, the first droplets of a thick and viscous fluid from the nipples can start to stand out at the very beginning of the baby's term. In some, colostrum is produced shortly before birth. There are even those women whose colostrum first appears only after the baby is born.
The second stage of lactogenesis (formation of stable lactation) begins after childbirth. Thick and yellowish colostrum over 2-5 days gradually becomes more liquid and turns into transitional milk. And only after this, during the third stage of lactogenesis, the mammary glands begin to produce regular breast milk.
Colostrum compared with breast milk has many advantages: it is more saturated with proteins that the baby can easily assimilate, it has a rich immune factor - antibodies that help the baby’s immunity to adapt to life outside of his mother’s womb, and resist the viruses and bacteria that surround every person on planet earth.
In vain the newly-made moms survive, believing that their baby stays hungry in the first few days before the transitional milk appears. Colostrum - very nutritious and fully covers all the energy needs of the body of the baby.
There is a popular belief that decanting a small amount of transitional milk enhances lactation and contributes to a faster “arrival” of constant milk in sufficient quantity. And what to do with colostrum after birth, many women do not represent. Let's see if it makes sense to express it.
Strain or not?
During pregnancy, expressing and squeezing colostrum is strictly prohibited. The mechanical effect on the nipples causes the release of the hormone oxytocin, which “brings” the smooth muscles of the uterus to full “alert”, the tone rises, preterm labor can occur, placental abruption can occur. Therefore, before delivery, the question of pumping should not be raised.
It should be noted right away that a large amount of colostrum during pregnancy does not guarantee at all that there will be a lot of breast milk, just as the absence of colostrum does not mean that there will be no milk or there will not be enough milk. Such a pattern does not exist.
Determination of colostrum after delivery, contrary to common misconception, does not affect the speed of lactogenesis processes. Therefore, it is not required to express it. The only exceptions are cases when a woman cannot put a baby on her breast in the first hours and days after birth.
Determination of colostrum makes sense if:
- the child is in intensive care, it is not brought for feeding due to its weak and painful condition, the colostrum needs to be decanted so that the lactogenesis process is not inhibited;
- the child was born weak with poorly developed sucking reflex; In order to “get” colostrum, the baby needs to try hard, and such children get tired quickly (expressed colostrum in this case is given to the medical staff so that the baby can take it from the bottle);
- giving birth was hard, a large number of drugs were administered to the woman, including antibiotics (especially the ototoxic Gentamicin, Neomycin and others); If the mother’s body has a lot of medications, the doctors themselves can recommend that she refrain from breastfeeding for several days, until the drugs are taken out with urine, then;
- during pregnancy a woman with a negative Rh factor had a high antibody titer; pumping should be done until the doctors determine the baby’s blood group and rhesus, and also make sure that he does not have hemolytic disease (in this case breastfeeding is allowed, if the disease is detected, the decision on breastfeeding is made individually);
- there was a big break between feedings (mother or child was taken away for examination, feeding was missed due to transfer to another hospital, etc.), “stagnant” colostrum must be drained;
- the child refuses to breast for various reasons (anatomically uncomfortable nipple, too strong nipple, the child is accustomed to eat from a bottle, etc.); There are many ways to "defeat" a stubborn person, to solve the problem of establishing breastfeeding, but temporarily it is worth resorting to the expression of colostrum.
All the other moms (and their 90% or more) do not need to decant the colostrum. These are extra efforts, additional experiences, besides the expressed colostrum is not stored for a long time even in the refrigerator, and therefore it is completely unwise to “stock up” it for the future.
How to do?
It is advisable to prepare for the expression of a woman, as far as the conditions of the obstetric institution in which she is located allow. You need a small capacity for decanting (for example, a plastic cup with a wide neck and thin walls). Capacity must be clean. If there is no boiling water for sterilization in the ward, ask the relatives to buy and bring a small convenient sterilizer for bottles and nipples, it is easy to handle the tank for squeezing. It works from the usual electrical network.
Before decanting, be sure to wash your hands - the process is carried out exclusively with clean hands. The mammary glands should also be washed with warm water and baby soap to prevent the penetration of pathogenic bacteria into the microcracks of the nipple. A napkin or a small towel that a woman will use to wipe her hands and soak up the drops of colostrum should be clean and ironed.
Strain the colostrum for the first time, if there is no relevant experience, the staff of the maternity hospital will help. Do not be shy to ask for help. For manual pumping you need a certain skill, and with it no one has ever been born.
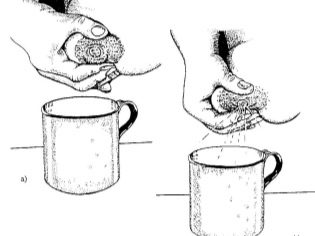
To begin pumping, place your thumb over the nipple and place your index finger under it. Pulling the squeezed nipple with your fingers is not necessary, it is correct - to press on it with progressive movements towards the sternum. If this is accompanied by pain, then something is done wrong. Try a more comfortable grip on the nipple with your thumb and forefinger and repeat the movement again.
Colostrum in women after childbirth is not so much to express it with a breast pump, and not everyone, judging by the reviews, such a device is convenient. But the most common medical disposable syringe is quite convenient. If he has a sharp nose cut off on the opposite side of the piston, then a convenient pumping device is obtained. The nipple is placed inside the cut-off part with the piston closed, it is checked how tightly it is there, whether it passes air.Then pull the piston in the opposite direction from the nipple.
Squeeze the colostrum and transitional milk into the syringe should be with great care, slowly withdrawing the piston to eliminate injuries to the nipples.
This method is definitely not suitable for stagnation ("stone chest"), with very thick colostrum, as well as for the first decanting (if the breast is not yet developed, such pumping into the syringe is traumatic, it is better to start by straining) manually.
After cesarean section
If the birth was performed surgically, then usually the change of stages of lactogenesis is somewhat delayed. The appearance of milk after cesarean section usually has to wait a little longer than after the natural generic process.
Self pumping after surgery does not represent a danger to the health of a young mommy. On the contrary, it stimulates the production of oxytocin, which will more intensively reduce the smooth muscles of the uterus. This will allow a woman not only to establish lactation, but also to avoid the common problem of operated women in labor - stagnation, poor uterine contractility, adhesions.
Before you begin pumping, be sure to talk about this with your doctor. He will tell you how best to organize this process so that mom and baby get the maximum benefit.
You will learn more about whether to callus callus after childbirth, you will learn from the following video.