Dr. Komarovsky about the treatment of chalazion in children
Despite the fact that chalazion is a predominantly age-related disease, peculiar to people of 35 years and older, it is sometimes diagnosed in children. And in this case, the question arises, where do ugly formations in the inner age come from and what to do with them. This question has to be answered both by Dr. Evgeny Komarovsky and his wife, the pediatric ophthalmologist Ekaterina Komarovskaya.
In this article, we have collected the most detailed answers to parental questions about child chalazion.
What it is?
The name of this pathology is not as common as rhinitis or bronchitis, and therefore most of the parents have no idea what this is about when they hear the word "chalazion". And we are talking about the formation on the inside of the upper or lower eyelid nodules, small formations, which at first parents take for barley.
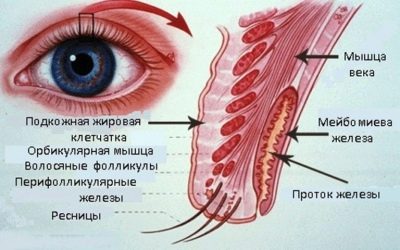
Barley is a purulent inflammation, it always flows only in the acute form. Halyazion is always a chronic disease. What happens in the eye of a child? The eyelid inflamed around the meibomian gland only if it is blocked and the secret produced by it accumulates in it.
Glands with such a complex name are located in the thickness of the cartilage tissue, and their exits just fall on the inside of the century. In each eyelid (lower, upper, on the right and left eyes) up to 70 meibomian glands are located. They are responsible for the secretion of the lipid layer of the tear film.
If the lacrimal glands produce a tear to moisten the eyeball, then the meibomian gland has the mission to develop lipids to prevent the rapid evaporation of the tear fluid.
If one of the glands is blocked, a lipid “gradient” is formed, which is called “chalazion”. The problem is widespread in people after 35 years, the elderly. In pediatric ophthalmology is not as common.
Causes
Accurately answering the question of why a child has a chalice, no doctor can, because until the end of modern medicine are not known the reasons leading to blockage of the meibomian glands. Therefore the main reason is officially considered the blockage itself.
Inflammation around the occluded gland and the lipid filling of its duct itself is a novelization, which is classified as benign.
What can lead to blockage is a difficult question. Some experts believe that "Trigger mechanism" are the preceding barley, especially if they were not completely cured. Also associated with the development of pathology factors oily skin, diabetes, blepharitis are considered.
Scientists even managed to find a connection between the occurrence of chalazion and diseases of the gastrointestinal tract and intestinal dysbacteriosis.
It is also believed that the appearance of ugly nodules in the inner eyelid contribute to stress, feelings, viral infections, lack of vitamins in the dietas well as improper use of contact lenses.
How to recognize?
Parents can easily recognize this pathology, because it manifests itself quite characteristic - on the inside of the eyelid appears a rounded dense tumor. It differs from barley in that touching a “hail” does not cause pain, and there is no pain when blinking.
Child's vision does not suffer from the presence of chalazion. With the growth of education (and it can increase to 4-6 mm), the defect becomes noticeable when you look at the face, without turning the century. The skin begins to swell, which also does not affect the function of the organs of vision. If the inconvenience is, it is only cosmetic.
Rarely, the chaliasion interferes - there are cases when the “headers” were the cause of increased tearfulness of the eyes, as well as itching. But this does not mean that you can leave a benign education alone with a clear conscience.
If nothing is done, the chalazion can continue to grow, and then pressure on the cornea can cause astigmatism. If the chalazion exists for a long time and is not opened, it can become a cyst.
Also, the “hail” can become infected with bacteria, and then signs of suppurative inflammation will appear: pain, swelling, perhaps even an increase in body temperature.
What should parents do?
First of all, Yevgeny Komarovsky and his wife Ekaterina advise to calm down and not panic. If there is any doubt, it is barley or, after all, a chalazion, do not be shy, you should contact an appointment with a pediatric ophthalmologist. This specialist will immediately find all the differences and after the usual visual inspection will be able to say with confidence what happened to the child.
Afraid to go to the reception is not necessary. Halyazion often does not require any other diagnostics except visual: instrumental methods that can frighten a child or give him discomfort are usually not used.
However, if the chalazions begin to appear with enviable regularity, then the doctor may need to conduct a detailed study to distinguish the chalazion from the dangerous meibomian gland adenocarcinoma.
For this purpose, a histological examination of the contents of the formation is prescribed.
How to treat?
To begin with, an ophthalmologist may recommend parents to wait a bit, because in childhood there are quite often self-healing cases - the chaladion passes without a trace on its own.
If you sit back parents unbearable, ophthalmologist may advise to bury disinfectant eye drops, lay anti-inflammatory ointment. Also, mothers can hold a century massage to the child. In the conditions of the clinic the child can attend a course of physiotherapy - UHF-therapy, eg.
Ekaterina Komarovskaya, an ophthalmologist specializing in the health of children's eyes, claims that dry warming has an excellent effect. A diaper warmed up with an iron can be applied to the affected by the chalazeus for five minutes three times or four times a day. But this method is definitely dangerous for children with signs of inflammation in the eye.
If the eye hurts, the chalazion itself is inflamed, warming up will only contribute to the spread of inflammation.
If the chalazion is long and progressive (growing), lasts for more than half a year, in the conditions of a medical institution, the introduction of cortexteroid hormones directly into the chalazion itself can be recommended with a thin needle. From the action of hormones, it resolves.
There are also surgical methods in which, under local anesthesia, the meibomian gland ducts are cleaned by the surgeon, the “granule” of the chalazion is removed entirely, along with the inflammatory “capsule” surrounding it.
After surgical treatment of the child, a tight bandage is applied to the eye. Recommendations on the use of anti-inflammatory ophthalmic ointments and drops are also given.
You should not be afraid of the wording “surgical excision”. Medicine is able to offer little patients not only a traditional surgeon’s scalpel. Today, surgery to remove the chalazion laser.
In such an operation, the content of the “gradient” is removed without cuts - using a laser beam.This is a less traumatic procedure with a simpler and easier recovery period, as the laser lid is not stitched to the inner eyelid during laser surgery.
The main advantage of laser surgery for chalazion is the lack of probability of relapse. After a normal operation, the likelihood that the lipid formation in the inner eyelid will appear again and not one, exists.
But before parents start to think about the benefits of a particular type. Chalazion removal, Ekaterina Komarovskaya and Evgeny Komarovsky recommend taking the following measures:
- apply dry heat for five minutes three times a day;
- twice a day to clean the edge of the eyelids from the rather fatty lipid secretion of the meibomian gland and dirt — use a solution of baby shampoo for this (“without tears,” of course).
If after half a year the chalazion failed or it grows and grows in size, parents should return to the ophthalmologist. and this time to discuss more serious methods of ridding the child of an ugly benign education.
Forecasts are very favorable. Most often, children absorb education independently without the help of doctors and parents.. In other cases, the pathology is well treatable.
If the capsule of the chalazion was not completely removed, then it is possible that there will be a relapse. Cases of complications, such as the formation of an abscess, phlegmon, and cysts or fistula at the site of the chaliasion, are not more frequent than in one out of ten people with such a diagnosis. And this one out of ten, as a rule, belongs to the category of children to whom parents tried to remove the “grading” on their own (there are, alas, those who believe that the best treatment is to squeeze, pierce and smear with ointment with antibiotics).
It is strictly forbidden to touch a lipid neoplasm on your own, to try to remove it mechanically.
Prevention
Since the true causes of the chalazion remain unknown, it is not possible to develop preventive specific recommendations. Therefore, parents should pay attention to the child's compliance with general guidelines for the health of the organs of vision.
Since the meibomian gland can become clogged with dirt, it is important to teach your baby to never rub his eyes with dirty hands, especially on the street and in the sandbox.
Such illnesses that are common in childhood, such as barley, conjunctivitis, blepharitis, should be treated in time and correctly. If the child wears contact lenses, you need explain to him the hygienic rules that are strongly recommended to remove and put on them with exceptionally clean hands, and store - in a special solution.
And, of course, you need to do everything to strengthen the child’s immunity. With strong immunity, the child is not afraid of inflammation around the meibomian gland, the body can easily cope with it, and even if a blockage occurs, it will quickly heal itself and go away without a trace and need for treatment.
In the next video, Komarovsky talks about other possible eye problems.