Breastfeeding after cesarean section
Breastfeeding after a caesarean section is considered to be an extremely difficult task and always associated with difficulties and problems. In fact, the effect of operative labor on subsequent lactation is somewhat exaggerated, although a great deal will depend on how young a mother will be able to properly establish the process of breastfeeding a baby. In this article, we will look at the features of milk production after cesarean section and show how to adjust feeding.
Special features
The mammary glands during pregnancy almost doubled in weight. Under the action of certain hormones (progesterone, estrogen), the milk ducts grow, the lobules become heavy, and only a couple of days before the onset of labor is the maturation of the glands complete. The drop in progesterone levels, common to all women before childbirth, triggers the mechanism for the production of immature milk and in the mammary glands.
But a caesarean section is not always done on the expected day of labor, and they do not always expect the body to be fully prepared for labor. It is for this reason that lactation may occur with a slight delay after surgical delivery, because hormonal adjustment requires some time. The speed of milk production is also influenced by the preparations that are used during the operation for anesthesia. They somewhat slow down the natural processes in the female breast.
It is clear that the closer to the date of delivery, a cesarean section was performed, the less problems the puerperal woman will have with lactation. If there was a premature caesarean section for health reasons and the readiness of the mammary glands is far from optimal, problems with milk production arise more.
For a successful start of feeding, the level of a particular hormone substance prolactin in the female body is important. To stimulate its production, it is important to attach the baby to the mother’s breast as soon as possible. Today, when up to 90% of surgeries are performed under epidural or spinal anesthesia, when a woman remains fully conscious when the baby is removed, breastfeeding in most maternity homes is practiced right in the labor hall.
Problems are likely in the event that it was not possible to immediately attach the child to the breast, if in the first 24 hours a woman is in intensive care in a serious condition or the baby is in a serious condition in pediatric intensive care. In this case, neither of the joint stay of the mother and the baby, nor of the delivery of the child for feeding is out of the question.
But even if all of the above negative factors occurred, this is not a sentence. Promoting the establishment of normal lactation is quite possible. There is no opportunity to feed the baby only in women who have no milk and colostrum due to hormonal disturbances, and such violations (of the prolactin type) are extremely rare.
What to look for?
The first and a half hours of his life in this world are considered to be the best time for putting a child to the breast. Nothing that milk is not yet fully understood, even a drop of colostrum will be quite enough for a crumb to get a large supply of proteins, vitamins, fats and carbohydrates. The nutritional value of colostrum is incredibly high. But even if there is no colostrum, it still makes sense for the crumb to attach to the chest for one and a half hours.
This will help the formation of its sucking reflex, will have a beneficial effect on the contraction of the uterus after the operation, and will also be an excellent stimulus for the production of prolactin. Not every maternity hospital is trying to hold in the first one and a half hours, but because this issue needs to be solved with the doctors in advance, agree on the time of application, if unforeseen circumstances do not occur.
Feeding mixtures is not the best start of nutrition. After the baby sucks the nipple, from which the food flows relatively easily, without resistance, he may then refuse to take the breast, because the baby will need to make some efforts to dissolve it. This question also needs to be discussed in advance with your doctor. A woman has the right to demand the absence of complementary foods on the first day. It will be introduced only if even the colostrum does not appear within 24 hours.
Today, long-term separation of mother and baby after surgical birth is not accepted. If there are no contraindications from the health of the mother and the baby, after 8 hours, when the woman starts to get up, they can bring the child for joint stay. From now on, the main measures for the formation of lactation will begin. Attaching to the breast will benefit both the woman and her child.
How to make milk production?
You should not worry if there is no milk on the first day or two after the operation. This is perfectly normal; in many women, after a cesarean section, even the colostrum begins to stand out late. Repeated people start to breastfeed earlier, because their nipples are more adapted to this and there is a corresponding experience. If the birth was the first, then the chest is still to be developed. It is this woman and will have to do in the maternity ward after the child is transferred to a joint stay.
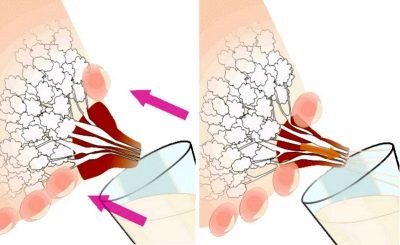
Increases milk production by pumping. It should be carried out every 3-4 hours to stimulate the production of complete breast milk. Even if all the efforts of the puerperal rested only in the production of a couple of drops of colostrum, you should not leave this occupation. You can cross the chest with your hands in the intervals between feeding the baby (by applying to the breast), you can use the breast pump.
There are several types of such devices - manual, pump, electric. Which one to choose is a personal affair of each mother and a question of the family budget. The principle of action is the same for everyone - the nipple is irritated, the production of prolactin is stimulated, the volume of breast milk increases. To strain the breast to a condition suitable for feeding the newborn is quite realistic within 2-3 days.
If the child does not take the breast, you need to find out the reason. It is mandatory to consult with a doctor from the children's department. It is possible that the nipple of the mother is small, anatomically uncomfortable. In this case, you may need a special silicone pad on the nipple.
If the milk is already enough and the baby eats well, you still need to continue to express the excess. The baby will grow and his nutritional needs will increase every day.
If breast milk residues are removed from the mammary gland, then the inhibitor, which slows down the production of a new portion of breast milk, will be eliminated in a timely manner.
In addition to pumping, there is a whole range of measures that will help a woman after surgery to establish breastfeeding.
Massage
Receiving a special lactation-stimulating massage is not difficult. They are under the power of any woman. Properly made massage will not only stimulate the production of milk, but also help to prevent its stagnation in the mammary glands.
Take the breast in the area of the upper part of the gland and with an open palm make circular movements from top to bottom towards the nipple. Five minutes to massage one breast, go to the second massage.
Light massaging of the nipples with a slight pressure with the tips of the fingers also helps. Massage each nipple clockwise and counterclockwise for 1 minute.
Massage should be done 4-5 times a day after each feeding.
Medicines
There is a separate group of drugs that can help establish lactation after surgery. Before use, you should always consult with your doctor, because in addition to benefits, they can also have side effects. The most popular with nursing mothers are such tools.
- "Laktogon" - 1 tablet 3-4 times a day for an hour before feeding the child. General course - 30 days.
- "Mlekoin" - five granules dissolve half an hour before meals in the morning and evening. Duration of treatment is unlimited, the drug is homeopathic.
Special nursing mixes can also help - “Milky Way”, “Femilak”. Taking folic acid is also recommended. If a woman has hormonal problems that interfere with the establishment of normal lactation, she will be prescribed hormones.
Nutrition
Meals should be balanced, but not scanty. On the first day or two, a strict diet is recommended to the woman after the operation; on the 4th day she can eat everything that is provided for at the common table for nursing women. The main thing is to prevent the occurrence of constipation. If there are difficulties with defecation (it is terrible to hurt, the seams hurt), you need to take a laxative in the form of rectal suppositories or microclysters to gently clean the intestines from the feces.
Porridges, milk, dairy and fermented milk products, steamed and boiled vegetables will be useful, it is recommended to drink more liquid. Women after the operation need the liquid doubly, because it is necessary to replenish the reserves of lost fluid, but you should be very attentive to your well-being, because stagnation and swelling of the mammary glands are not excluded due to the large amount of drinking.
You can add to the diet special teas for nursing mothers with fennel, they will help enhance the production of breast milk.
Medication Effect
Often, women after surgery wonder how drugs that make the puerperal in the postoperative period can affect the baby. It should be noted that pain relievers are administered to the woman for the first 2-3 days, since uterine contractions with sutures placed on her can be quite painful, and the anterior abdominal wall is quite noticeably disturbing. Separately administered drugs are introduced, since the contractile ability of the uterus after surgical delivery leaves much to be desired. These drugs will not cause harm to the child.
Antibiotics are prescribed today only if there is reason to suspect infection. Just so, for the prevention, as was done earlier, antibacterial drugs are not prescribed after a cesarean section. Modern drugs for the most part are not dangerous for the child, but if a woman is prescribed a fairly toxic antibiotic, she will be warned about it.
At the time of therapy, breastfeeding will have to be abandoned. So that the milk does not disappear and it was possible to feed the baby then, the woman will need to continue to decant and massage her breasts.
«Contractubex», Which many women use on the scar area after its healing, does not affect breastfeeding if the drug is used in the form of a patch. The effect of the gel on the composition of breast milk has not been studied sufficiently, but because manufacturers do not recommend nursing mothers to use the product in this form.
Useful tips
Develop a feeding regime that will be convenient for both mother and baby. Tips to apply a crumb to the breast more often after the operation can turn into other problems - a crumb in a couple of months will “hang” around the clock on the chest, which will give him and his mother a lot of inconvenience.
If the baby is used to bottle feeding in the hospital, then the mother will have to try to retrain the baby.In this case, a rational approach will be in hourly feeding, in which the child will get used to food at certain hours, and female lactation will “fit” as well as possible to the needs of the child.
Caesarean section is not a cause for fear of lactation and the success of breastfeeding. There is nothing irresistible on this path. Women who give birth naturally have sometimes no less lactation problems than those who have given birth by caesarean section. It all depends on the focus of the woman on breastfeeding, on her understanding of all its importance for the growing child. As a last resort, at every antenatal clinic there are experts on HS, you can ask for advice absolutely free of charge at any time.
For information on how to establish breastfeeding after cesarean section, see the following video.