What is a spermogram, and what does it show? What to do in the presence of pathological forms?
When a married couple cannot conceive a child, many believe that the reason lies in the state of health of the woman. In fact, this is not always the case. About 40% of cases are male infertility. That is why a survey on the inability to get pregnant should pass both spouses.
The complex of examinations for a woman is large and time consuming. It is sometimes enough for a man to simply pass a sperm sample for semen. In this material we will describe how this analysis is carried out, what its norms are, how to decipher the result and what to do if the actual results are far from ideal.
What it is?
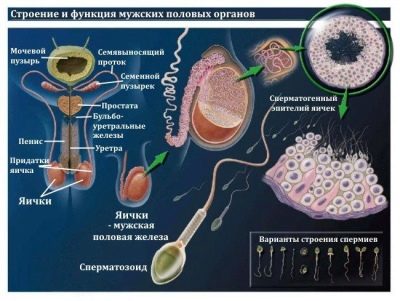
If the word “spermogram” is decomposed into two Greek roots (“sperm” - σπέρμα and “gram” -γρμμα), then this medical term will literally mean “seed record”. In fact, it is a laboratory study, the analysis of sperm, which allows you to find out how suitable it is for fertilization of the female egg.
The analysis makes it possible to find out some quantitative and qualitative indicators of male sperm, which gives the doctor, who carries out diagnostics, the opportunity to ascertain whether family infertility is male, whether the man has diseases of the reproductive system.
The study is assigned not only to the representatives of the stronger sex, whose wives cannot get pregnant or suffer from habitual miscarriages or miscarriages, but also to men who are preparing to become sperm donors, as well as men who would like to freeze their sex cells for the future (cryopreservation is recommended for those at a young age, he goes on military missions dangerous for life, works on objects with an increased level of radiation and is in other circumstances that may adversely affect the ability of the m have children in the future).
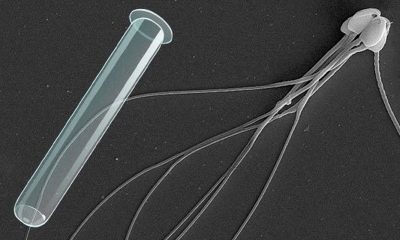
The first spermogram in the history of mankind was held by the legendary scientist Leeuwenhoek, the creator of microscopes, back in the 17th century. True, his research was superficial. He only drew attention to the fact that a number of representatives of the stronger sex cells in the ejaculate move more actively than others. It took humanity about 300 years to formulate the theses.
Only at the beginning of the 20th century were unified requirements for quantitative indicators of male seminal fluid. They were revised several times by the World Health Organization, and recent changes were made to the analysis in 2010.
All over the world, semen standards do not cause any doubts. However, Russia has developed its own practice, different from the world. So, only part of the laboratories that can examine the seminal fluid, operates according to WHO standards.The rest have their own standards and requirements, as well as criteria for assessing and understanding the pathology and rate.
Therefore, we wanted to start this article with one important wish. Before comparing your sperm results with the WHO guidelines below, specify in the laboratory where the analysis was conducted, whether it works according to these standards. If not, then you can ask about the specific rules of this laboratory.
Experts in reproductive medicine are confident that in the near future all Russian laboratories will switch to world standards, but this will be later.
Why the analysis is carried out and how to take it?
Spermogram is needed in order to find out how high fertility a man has, that is, the ability to fertilize. A study under the microscope. The diagnostician determines the quantity, quality and some other properties of sperm.
Sometimes there is a need for additional tests, such as the MAP test, which allows you to identify specific immunological processes - the production of antibodies to sperm. Sometimes the doctor requires data on the biochemistry of the ejaculate, in order to understand the genetic value carried by the spermatozoa, a spermogram is carried out with DNA fragmentation. The analysis is prepared in different laboratories in different ways. On average, it takes from 1 to 3 days, but it happens that the terms are delayed, for example, if genetic testing is required.
For the results to be reliable, the man should know the rules by which the analysis is done. They concern the observance of recommendations before the surrender:
- For 3-6 days a man should limit sex and not masturbate. During this time, it will have time to mature enough germ cells to imagine their average number. It is the specified number of days that you need to abstain before donating sperm, because prolonged abstinence also negatively affects the composition of the ejaculate; after prolonged abstinence, the sperm is thick, sticky, which makes it difficult to study.
- A week before putting the man should refrain from sunbathing and visiting the solarium, from going to the bath, sauna and any thermal effects on the genitals. Seat heaters in the car also should not be included.
- A week before delivery, you should not take alcoholic beverages, and especially drugs, a lot of smoking. It is advisable to refuse to take medication, but if this is not possible, it is better to postpone the analysis to another time. The effect of antibiotics, hormones and other drugs on sperm quality can be devastating.
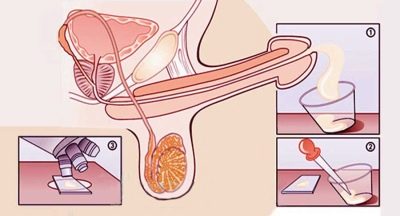
- Usually the analysis is passed by masturbation. This can be done both in the clinic and at home, where a man is psychologically easier and more familiar. In the clinic for collecting ejaculate issued a special container for biomaterials. For home gathering, such a container or a medical condom without lubricant and foreign substances can also be issued, in which a man can have normal full sexual intercourse with a partner. The most preferred fertility doctors consider the first method in which a man is tested in a clinic in a special jar.
- Collected by any of the methods of ejaculate, it is important to deliver to the laboratory as soon as possible - it is desirable to do this within 1 hour. When transporting it is important to remember that the seed must be at a temperature close to the body temperature. To do this, you can use a special thermal container. You can buy it at a pharmacy or get it at a clinic with which you have an examination contract.
Check the quality of sperm at home is impossible. But you can suspect pathology by conducting a home test. SpermCheck. The test and instructions for it can be purchased at the pharmacy, conducting is not much more difficult than a normal pregnancy test. However, the test system determines (not too, by the way, exactly) only the number of spermatozoa in the ejaculate (approximately).
Male infertility can be connected not only with quantitative disorders, but also with qualitative ones (there are abnormalities in the structure of germ cells, there are deviations in functionality), and therefore there is no alternative to spermogram.
What shows?
Spermogram gives an idea of the microscopic and macroscopic features of the germ cells of a given man. All parameters that are evaluated in the laboratory according to WHO standards are presented below.
Quantity, volume
This indicator is very important not so much for determining the level of fertility as for the correct conduct of all laboratory manipulations with the ejaculate. It is measured with a special pipette with a graduated wall. It also determines the viscosity of sperm.
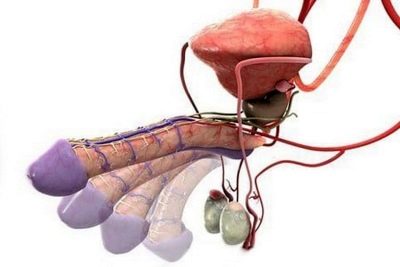
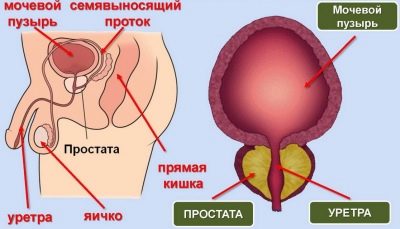
For a normal study, at least 1.5-2 ml of semen is required. The volume depends on the amount of specific fluid that the seminal vesicles and prostate gland produce.
Insufficiency of fluid may indicate problems with these parts of the male reproductive system. The shorter the period of abstinence, the less sperm is released.
Liquefaction time
Sperm tend to liquefy, become more fluid as it passes a certain time from the moment of ejaculation. This time is called liquefaction time. It is different for all men, significant fluctuations - from 15 minutes to an hour. Sometimes with certain pathologies sperm cannot be diluted at all.
Viscosity is determined by the length of the "filament", which remains when the laboratory glass rod touches semen when the instrument is lifted. If it is more than 2 centimeters, the sperm is considered to be viscous.
Special protein provides immobility and inactivity of spermatozoa while they are in the male sex glands. Under the action of the juice of the prostate gland, the protein dissolves, the “zhivchiki” become active and mobile.
If liquefaction does not occur, the doctor will suspect the pathology of the prostate gland. To dilute the sperm in the laboratory help some enzymes that are added artificially to assess other parameters.
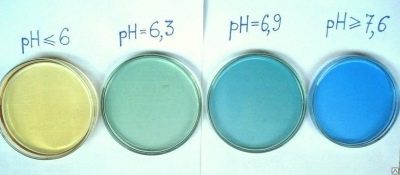
Acidity level
This indicator is determined by special indicators of paper or a special device: the pH of a healthy man is above 7.2. Insufficient acidity reduces the ability of sperm cells to dissolve the shell of the egg when introduced, thus, fertility decreases.
Smell and color
The smell of infertility is not judged. This parameter has no special diagnostic value at all, however, it is still indicated in the conclusion about the spermogram performed, which causes a lot of questions for the spouses and gives rise to many myths about the connection between the smell and the fertile ability of the man. There is no connection.
They indicate that the smell is “specific” solely by tradition, by habit, because it has always been this way. Pay special attention to this parameter.
The same dubious parameter is considered and the color of sperm. It is believed that in a healthy man, it should be white or grayish. Pink, yellowish, greenish shades can speak about pathologies - admixture of blood, pus. However, the spermogram fairly accurately answers the question of the presence and absence of substances at the cellular level, so there is no need to separately evaluate the color. It is indicated, like the smell, to a greater extent as a tribute to medical traditions.
In fairness it should be noted that the smell of semen gives a special enzyme - spermine. Its functions in medicine and science are not yet known. But some doctors say that the smell can be used to judge the health of the prostate gland, which produces this spermine. There is no official evidence for this method of diagnosing prostate problems.
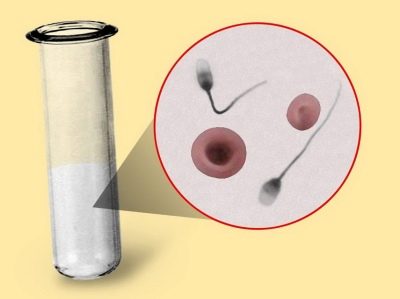
Sperm count
The number of germ cells laboratory assistants counted in 1 ml of fluid, as well as in the entire volume of the ejaculate completely.Do not think that they consider people to be "alive". It would be impossible, because in 1 ml there are millions of them. Calculations make special counting chamber.
In order to speed up the process of mathematical calculations, a laboratory technician can apply sperm on a glass of 22x22. In a drop of sperm on such a piece of glass with an increase in the microscope by 400, the number of cells that will speak about the number of cells in 1 milliliter will appear in the field of view. For example, a laboratory technician will see 20 cells, this will indicate the presence of 20 million cells in 1 ml.
In some laboratories there are sperm analyzers - special microscopes with an integrated camera, which themselves record and count the number of germ cells in the seminal fluid. In the event that there are few spermatozoa, and it is possible to see only single tail representatives in the field of view of the microscope, the sperm is placed in a centrifuge and the number of cells in the sediment is studied.
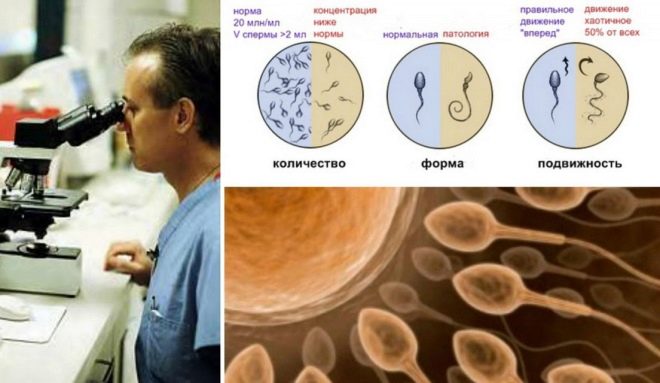
Total cell motility
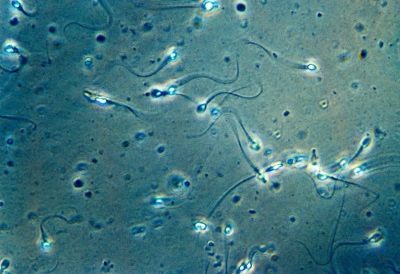
According to their ability to move and ultimately reach the cherished goal - the eggs, all spermatozoa are divided into 4 groups, designated by capital Latin letters from A to D.
The most persistent and goal-oriented cells are category A. Doctors describe them as progressive, active and mobile. Such germ cells move only directly and fairly quickly, at a speed of 25 micrometers per second. That is, in two seconds such selective “livelivers” manage to overcome a distance that is equal to their own growth.
Category B sperm differ from their elite comrades only in speed, it is slightly lower. But the direction of movement they have, too - only straight and not a micrometer to the side. It is believed that only spermatozoa with a mobility category of A and B are able to fertilize the female reproductive cell.
Category C cells may behave differently. Either move in one place, or move erratically, not in the forward direction, in circles, zigzags, etc. They are called non-progressive and mobile, and such sperm cause no particular hope for fertilization.
"Zhivchik" the latter category D does not move at all.
For conception it is important that the semen of the future dad was at least a quarter of germ cells of category A. If this amount is less, the laboratory technician evaluates them in total with the “colleagues” of category B.
A healthy spermogram will be considered such a result, in which a man's semen will show up at least 50% of “zhivchikov” category A and B in total.
The ability of germ cells to move is also monitored by sperm analyzers or counting chambers. This occurs simultaneously with the counting of their number.
Sperm morphology
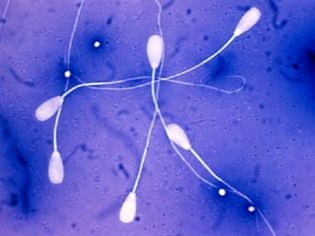
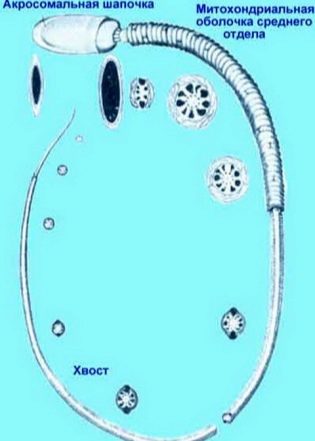
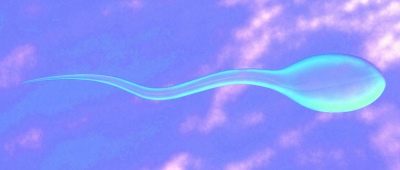
This is an extensive study of the structure of sperm. Microscopically, the doctor examines how the male sex cells are folded. Evaluated the shape and structure of the head, neck, middle part, tail, the appearance of sperm.
Most often, Kruger's strict criteria are used, by which the structural features of the cells are compared with the standard, and any boundary value belongs to the category of pathology, the cell is rejected.
The sperm head must be in the singular, flat and oval. It should not be squeezed, conical. Head dimensions in length - 4-5.5 microns, width - 2.5-3.5 microns.
Particular attention is paid to the acros in the head structure. There should not be vacuoles in it, it should occupy about half of the head area.
The sperm neck should be flat, small, not more than 1 micron. It is important that it is tightly and securely connected to the head, eliminating the likelihood of tearing off the tail. The connection should be at right angles.
The tail or flagellum is the longest part of the male sexual cell. It should occupy not less than 90% of the length of the entire spermatozoon. The tail should be one, even, slightly tapering towards the end.Twisted tails, flagella short or broken off, as well as pathology of the head, the middle part of the cell are the basis for rejection.
Do not think that a healthy man does not have defective sperm. They are always quite a lot. At various times, WHO recommended that morpho logical cell presence be the norm. ranging from 50 to 70%.
The Kruger criteria clearly state that the proportion of spermatozoa with defects can be up to 85%. Thus, for conception naturally, it is necessary for a man to have at least 14-15% of standard, ideal, perfectly healthy and morphologically correct spermatozoa.
Viability
This parameter indicates the number of live germ cells in the ejaculate. If the sperm cell is mobile, then it is definitely alive. But the fixed cell can be both alive and dead.
It is considered normal if not less than half of the living cells of different categories of motility (A, B, and C) are in the man's semen. The cells of category D are immobile, but it is necessary to investigate their vital activity only if the remaining living cells are less than 50%.
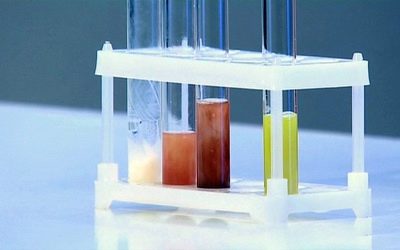
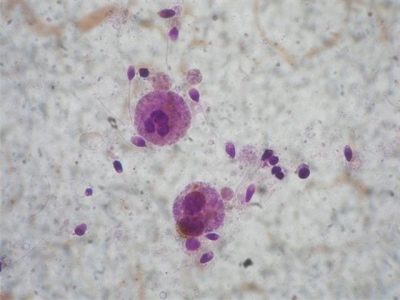
To understand whether the zinger is alive, assess the condition of its outer membrane. After cell death, the integrity of this envelope is broken. To the sample add the dye eosin. He can not get inside the living sperm with a whole membrane, but easily penetrates into dead cells, the shell of which is already broken. Such spermatozoa under the action of the dye become pink.
Another method is based on placing a semen sample in a hypotonic solution. Living and living cells at the same time begin to increase, swell, their tails begin to twist into loops, and the dead do not react in any way. With both methods, the result is assessed using a microscope.
Round cells
In addition to the caudate sperm, the male seminal fluid also contains other cells that are not sexual. They are called round or round. This mainly includes two types of cells - leukocytes and immature spermatogenesis cells.
Initially, the World Health Organization proposed to determine their concentration, believing that this might indicate, for example, an increase in leukocytes in semen. Later, the organization itself canceled its instruction, recognizing that the concentration of round cells does not have much diagnostic value. Some laboratories continue out of habit to fill in this spermogram blank column, but you should not pay attention to it.
Any man has immature cells that have yet to become sperm cells. Their number may vary, it is not constant, and the total concentration of such round cells is also recognized as uninformative. If it is determined, it is exclusively “by habit”.
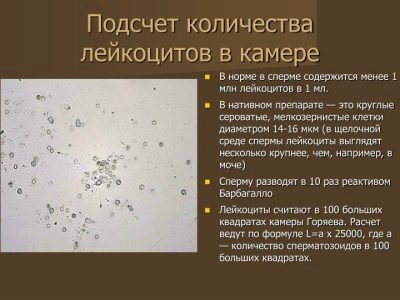
White blood cells
Leukocytes in the semen is at all. It is important how much their number is. If such cells are found more than 1 million in 1 milliliter of seminal fluid, then most likely the man has inflammatory processes in the prostate gland or seminal vesicles.
To identify leukocytes using the method of staining sperm and its subsequent examination under a microscope. Only in this way can leukocytes be distinguished from cells, which will soon become spermatozoa, but for the time being are rudimentary round cells.
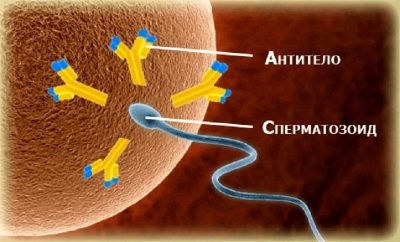
Antisperm antibodies
The male body, like the female body, can produce antibodies to sperm, and this will significantly complicate the task of conceiving a child, because immunity will simply destroy the male germ cells with special antibodies, regarding spermatozoa as a threat. Such immunity can develop with infections of the genital tract, with anal sex.
If the antibodies attack the sperm head, the germ cell will not be able to merge with the egg cell.If the tail of the sperm is attacked, the cell will lose its ability to move.
The presence of such destructive antibodies may be indicated by spermagglutination — the gluing of spermatozoids between themselves by the affected part — heads or tails.
Detect the presence of antibodies accurately allows MAR test during which a sample of rabbit antibodies against human antibodies is added to a sperm sample. If the drug, or rather the silicone microparticles that enter it, adhere to the spermatozoa, then it is very likely that this is immunological infertility.
Results OK - Transcript
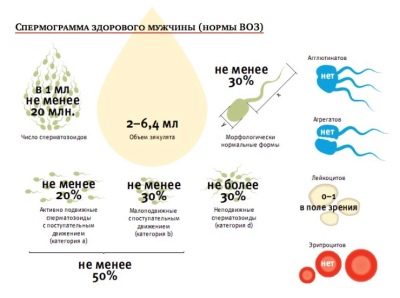
Good indicators of healthy semen are as follows:
| Main indicator | WHO standards after 2010 (current) | WHO standards until 2010 (for reference purposes) |
| Volume of ejaculate | Not less than 1.5 ml | Not less than 2 ml |
| Sperm acidity | Not less than 7.2 | Not less than 7.2 |
| Sperm concentration | Over 39 million in total, at least 15 million in 1 ml of material | Not less than 20 million in 1 ml., Not less than 40 million in total |
| Mobility | Not less than 40% of cells A and B, more than 32% of cells of type A | 50% of type A and B cells, or 25% of type A cells an hour after ejaculation |
| Viability | At least 58% of living cells in the sample | At least 50% of live sperm |
| White blood cells | Not more than 1 million per 1 milliliter | Not more than 1 million per 1 milliliter |
| Antibodies to semen | Not more than 50% of the test results | Associated with antibodies in the MAP test is not more than 50% |
| Sperm morphology | At least 4% of healthy cells | 15% of morphologically healthy cells, at least 4% |
Pathologies can be diverse, all of them are somehow connected with quantitative and qualitative deviations from the norms, as well as dysfunction of the male sex cells. Pathological conditions - description and causes
If no pathological forms are found in the spermogram, the doctor applies the term "Normozoosperiya", which means that the test did not reveal any abnormalities and the semen values are normal.
If pathological forms are found, then there may be quite a lot of names. We will tell about them in more detail.
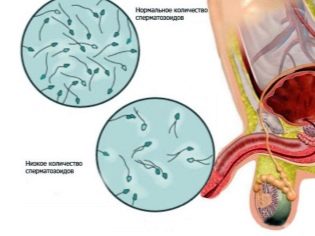
Oligozoospermia
This term refers to the pathological condition in which the number of spermatozoa in the ejaculate is significantly less than the existing standard values.
Both congenital and acquired causes may affect the concentration of germ cells. This can be as a complete congenital absence of the testicles, as well as having them, but not letting them into the scrotum (cryptorchidism). Often, the number of germ cells is reduced due to varicose veins, the varicocele.
Sperm count may be reduced due to trauma or inflammation of the testicles, due to chronic sexually transmitted infections (mycoplasma, ureaplasma, chlamydia, etc.).
If a man regularly overheats the scrotum, for example, is a great lover to visit the sauna or steam in the bath, working under high temperatures, then the number of germ cells in the seminal fluid may also be reduced.
The root of the problem may lie in the pathologies of the spinal cord, kidneys and liver, uncontrolled malignant smoking, drug use. The effect of alcohol on sperm count is also large, and if a man is abusing strong drinks, oligozoospermia is only one of several diagnoses that can be expected from the results of spermograms.
A decrease in the number of spermatozoa can be observed with defective, inadequate, irregular nutrition, with frequent stresses and heavy physical exertion, insufficient sleep, as well as with hormonal disorders, for example, with insufficient testosterone levels, and with frequent sexual intercourse. It is for this reason that men are advised to abstain from sex and masturbation before passing sperm for testing.
Asthenozoospermia
So doctors call the condition in which the sperm motility is impaired. They may be enough, but conception does not occur, since germ cells are simply do not get to the egg because of reduced activity.
The cause of the lazy behavior of the “zhivchikov” can be a violation of the morphology of the germ cells themselves, with some anomalies the sperm have no tails, or, on the contrary, there are two or more flagella, the head is reduced or enlarged.
Anomalies of sperm development may be congenital or acquired, which have become possible due to poor ecology, due to the improper lifestyle of a man.
The reason for the inability of sperm to actively move forward (dyskinesia) can be a high viscosity of seminal fluid. Increased viscosity is often observed in men who have sex too rarely, and also in men whose activity is associated with exposure to toxic substances and poisons. Violation of the ability of germ cells to move can be observed with advanced forms of genital infections, as well as prostatitis.
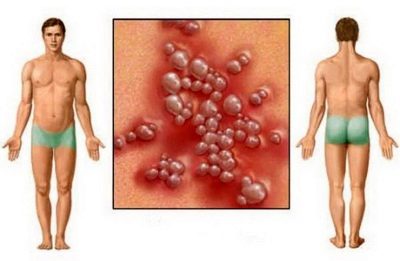
Teratozoospermia
This term indicates the presence in the sperm of a large number of ugly, mutated sperm, with morphological disorders - pathologies of the head, tail, middle part, neck. They can be not just the reason for not being able to get pregnant, but also the cause of miscarriages in women, the cause of gross chromosomal abnormalities in the fetus.
That is why it is important to assess the morphology of the male sex cells before pregnancy, so as not to state the sad facts during the carrying of the child or after the termination of the pregnancy.
The causes of abnormalities in the structure of germ cells in the representatives of the stronger sex can be hormones. If a man has a hormonal failure, the number of reference, ideal for conceiving germ cells in the ejaculate is significantly reduced.
Quite often, the morphology of sperm is violated in men who undergo hormonal treatment or use steroid hormones for sports, fitness, bodybuilding, weightlifting.
Mutated germ cells may be viral infections. The most dangerous of these diseases is a herpes infection of the second type, which is also called genital herpes.
An important influence is exerted by the excessive consumption of beer and other alcoholic beverages, nicotine, drugs, stress and lack of sleep, poor diet, lack of vitamins. Living in regions with unfavorable ecology or simply the conditions of a gassed big city is also a prerequisite for disrupting the sperm morphology.
Azoospermia
Behind this name lies a severe form of male infertility, in which there are no sperm in the ejaculate. If the pathology has an obstructive cause, then the sperm mechanically can not go out and mix with seminal fluid, for example, due to pathologies of the structure of the reproductive system.
Occlusion may occur in the epididymis or in the seminal ducts. The non-obstructive causes of the absence of germ cells in seminal fluid are associated with abnormalities in the production of sperm initially.
Azoospermia can occur as a result of severe inflammatory diseases of the reproductive system, both viral and bacterial. The disease can be inherited if the corresponding gene "plays" in the genetic set. For example, a complete absence of the vas deferens may be congenital.
The reason for the absence of spermatozoids may be in the injury of the testicles, in operations carried out on the spinal cord or liver.
Operation vasectomyin which the ducts intersect or overtighten, leads to complete sterility of the sperm, to the absence of sperm in the liquid, which is used as a means of surgical contraception.
The lack of “zhivchikov” due to violations of their production occurs often under the influence of antibiotics, drugs for the treatment of cancer diseases, after completing courses of chemotherapy and radiation therapy for cancer diseases.
Aspermia
This is the complete absence of sperm during orgasm or a very small amount of it. With true aspermia, sperm does not stand out completely, and there are also no bright orgasmic sensations at the end of sexual intercourse. With a false aspermia, men experience an orgasm, a small amount of ejaculate may even be released, but there is not a single spermatozoon in it.
The cause of this phenomenon may be retrograde ejaculation, when the release of semen occurs in the bladder. Often, for a long time, untreated sexually transmitted diseases, inflammatory processes in the reproductive system of the representatives of the stronger sex create prerequisites for the development of aspermia.
Not the last place among the reasons for the absence of sperm is given to mental and emotional disorders, spinal cord and brain injuries, as well as congenital defects of the testicles and vas deferens.
Aspermia can be a complication of such a common disease, such as diabetes, tuberculosis. Often it is diagnosed in men who abuse alcohol and drugs. At an advanced age in men comes the physiological aspermia, it is considered irreversible. In all other cases medicine is ready to help a man to become a father, but specific actions depend on the root cause of the condition.
Leukocytospermia
Excess levels of leukocytes in seminal fluid are diagnosed as a fait accompli. The true cause of the abundance of white blood cells in the ejaculate is not always possible to establish. A large number of leukocytes destroys the membranes of sperm and reduces their ability to move.
The appearance of these cells in semen always speaks of an inflammatory process. But the location of the process is not always found, especially if the disease is chronic and is almost asymptomatic.
Often, white blood cells in excess of excess of the standards presented in the table above, appear in the sperm due to vesiculitis, prostatitis, urethritis and other inflammatory ailments. Therefore, with such a result, the spermograms will require an additional examination that is quite impressive in its scale, including tests for infections, urine counting and other diagnostic methods.
Akinospermia
In this pathology, there is complete immobility of sperm. They can be alive, contain normal genetic material, but they cannot reach their goal, the egg cell. Men can have immobile sex cells from birth, that is, his spermatozoa are already formed with impaired motor function, and can become immobile under the influence of acquired factors.
The reason for the production of such germ cells can be damage to the epithelium, which was accompanied by an infectious or inflammatory disease of the urogenital system, including venereal disease.
Motionless sperm can become with ankylosing spondylitis or rheumatoid arthritis. Cell motility can be completely lost due to significant excess sperm antibodies.
Necrospermia
With this pathology in the semen completely or almost completely no live sperm. If the problem is true, and the sperm are already being produced unviable, then medicine, alas, will not be able to help.
However, this form of necrospermia is an extremely rare occurrence. Most often in representatives of the stronger sex occurs partial or complete necrospermia, in which the death of germ cells occurs under the influence of some negative factors after development.
In the first place in terms of a killer effect on spermatozoa are sexually transmitted infections that are transmitted by intimate means. Further, there are hormonal disruptions, in which the level of male hormones in the body of a man is insufficient to maintain the life of germ cells.
Also, dead sperm can become in tuberculosis, renal failure, after injuries of the reproductive organs or radiation exposure. A prerequisite for the development of pathology may be varicocele.
Bacteria and viruses cause a decrease in sperm acidity, with the result that sperm cells, which are very sensitive to changes in their environment, start mass-massing within hours.
Spermatozoa are updated less frequently, the cycle of spermatogenesis takes 74 days. However, in the case of complete and partial necrospermia, doctors can help a man become a father.
Cryptospermia
Such a diagnosis is made after the spermogram is carried out using traditional methods and it showed so few spermatozoa that it was necessary to do centrifugation. Cryptospermia is a negligible number of germ cells in the sediment after passing through a centrifuge.
The cause of the phenomenon can be the mumps transferred in childhood (infectious parotitis), as well as varicocele, genetic pathologies of the reproductive organs and the reproductive system, hormonal imbalance. All causes, except genetic and congenital, respond well to medical correction.
Hemospermia
Such a pathology is indicated if blood is detected in the spermogram. Normally, there should be no blood in the ejaculate. True hemospermia is different from false in that blood enters the seminal fluid from the testicles, the prostate gland. And in case of a false type of pathology, it is in the form of a vein mixed into the ejaculate already in the urethra when passing out.
The cause may be prostatitis, urethritis, vesiculitis. Also, blood in the semen can be observed in some oncological diseases. In this pathology, unlike many other problems with sperm, there are symptoms, and the man will be able to notice them in time. This is not only a visual change in the color of sperm, but also pain when urinating, a decrease in sexual desire, a decrease in orgasmic sensations.
The reason may also lie in the frequent and intensive sexual contact, inflammatory processes, impaired blood supply to the reproductive system of the man.
Treatment and recommendations for improving sperm quality
The restoration of sperm quality can only be discussed after the causes of the pathological forms of the spermogram have been identified. Usually the treatment gives a good effect, and 90% of men with acquired pathologies manage to restore fertility.
If the cause lies in infections, and this is proved by laboratory tests (blood, swabs, urine), then antibiotic treatment is prescribed, in the case of herpes infection - antiherpetic drugs. An antibiotic is often prescribed. «Levofloxacin»related to broad-spectrum drugs.
After anti-inflammatory treatment, a man recommended a course of vitamins during the spermatogenesis cycle - about 3 months. This time is necessary to restore the quality and quantity of sperm.
Men whose causes of infertility are rooted in mechanical barriers to the discharge of sperm can be treated with a subsequent course of antibiotics to prevent the inflammatory process. Vitamins E, A, C, D, B, folic acid, minerals, especially zinc and selenium preparations, shown to all men with impaired quantity and quality of seminal fluid.
If the reason is non-infectious, then sometimes it is enough to change the situation - to live for several months not in an urban setting, but outside the city, in the fresh air.
Nutrition correction includes an introduction to the diet of protein products, milk, meat, fish, cottage cheese.A man, in order to increase the volume and functionality of the ejaculate, must comply with the drinking regime, give up bad habits and keep the mode of sexual activity recommended by the doctor (too frequent sex harms the quality of sperm no less than too rare sexual relations).
Improving the quality of sperm often occurs after a man corrects his work activity, refuses to work on the night shift, begins to get enough sleep, fully relax.
Weekend on the couch should be replaced by skiing or swimming, cycling, easy jogging.
If the cause of the pathological form of sperm lies in a hormonal failure or imbalance, endocrinologist prescribes treatment with hormonal corrective means. Simultaneously with this therapy, the necessary vitamin complexes for men are being taken.
If treatment does not help improve performance, then the reproductive auxiliary methods such as IVF and ICSI.
In the extreme case (and such a need arises only in the case of a genetic pathology in a man, an irreparable, total pathology of spermatogenesis) donor sperm may be required for fertilization. It would be a desire to have children, and the way modern medicine will tell.
Reviews
Men are quite reluctant to leave feedback on the passage of such a diagnosis on the Internet, but among them you can still find really informative. Firstly, most of those who have already decided on spermogram come to an amazing discovery in its simplicity - this is not scary, not disgusting, and not at all embarrassing. To be ashamed of this diagnosis is absolutely nothing.
Secondly, the results are exhaustive, and on their basis it becomes clear in which direction the couple should proceed further - start treatment or additionally check the health status of the female half of the family.
The analysis is not expensive, it can be done in any city, since many clinics provide such a service.
On how to properly pass the sperm, see the following video.