What is ICSI - intracytoplasmic sperm injection, how is the procedure?
When a couple cannot conceive a baby for a long time, but medicine cannot help them with medicines and other means, in-vitro fertilization is recommended. With IVF, the egg is fertilized outside the female body, in a test tube. If the merging of the sex cells of a man and a woman does not take place in the laboratory bowl, then it is too early to despair, because one of the methods of artificial insemination, ICSI, can come to the rescue. That this such and as such procedure is carried out, we will tell in this article.
Definition
The abbreviation "ICSI" is derived from the English "ICSI" - IntraCytoplasmic Sperm Injection, which literally means "intracytoplasmic injection of sperm." ICSI is a modern method of treating various forms of infertility, which allowed thousands of couples with complex forms of reproductive disorders to gain the joy of motherhood and fatherhood.
This method should not be confused with IVF as a whole or with artificial insemination. When intrauterine insemination fertilization occurs inside the female body, where it is provided by nature - in the ampullary part of one of the fallopian tubes. The sperm is simply injected through a thin catheter into the uterine cavity, which allows a greater number of male germ cells to survive and successfully reach the egg cell. In IVF, the egg is fertilized by sperm in a laboratory Petri dish. At the same time, sperm cells “storm” the oocyte membrane in almost the same way as they do in natural conditions with natural conception.
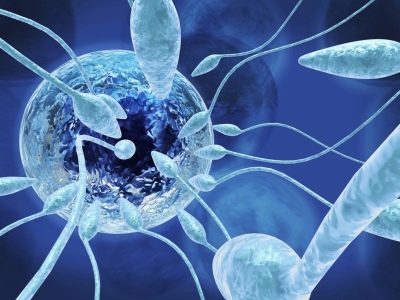
ICSI is required when spermatozoa are unable to fertilize an egg, even in the embryology laboratory, with all its nutritional compositions, by pre-cleaning the ejaculate from impurities and seminal fluid. Then the doctors make a real miracle, which requires a lot of experience and a certain “jewelery” from them - they inject the most healthy sperm cell with a thin needle directly under the egg shell, into its cytoplasmic fluid. Once at the right place, sperm has a better chance of fertilization.
With natural conception, insemination or IVF in the Petri dish, sperm have to overcome several obstacles - a radiant crown, a shiny egg shell, and only the most enduring can penetrate under the shell. ICSI allows you to "shorten" the path.
Russian doctors most often call the ICSI method with the shock last vowel, and only St. Petersburg doctors pronounce the first “I” when pronouncing the name of the procedure.
For the first time the method was used by Belgian doctors in 1992. Then, in the Brussels Center for Reproduction, they helped the couple in such a way to conceive a baby, which was unsuccessfully treated for infertility and even did several IVF for 20 years.
In Russia, the method took root a little later, the main contribution to its development was made by scientists from NIIAP - Research Institute of Obstetrics and Pediatrics. The first attempts to “manually” deliver sperm to the egg were made earlier, during Soviet times, when the first two successful IVFs were performed in Moscow and Leningrad in 1986.However, at that time, medicine did not have high-precision equipment that would allow to achieve accuracy at the cellular level.
Today there are such opportunities, the ICSI procedure is considered to be high-tech. It is held for medical reasons, which are stipulated by the Order of the Ministry of Health, stipulating the procedure for providing assisted reproductive care to Russians.
You can make ICSI both at your own expense and free of charge - according to a quota of regional or federal.
The procedure is carried out with the husband’s sperm, as well as with the donor’s sperm, if there are strict medical indications, or if the woman’s own will, if she lives alone, has no permanent sexual partner. Most often, ICSI is recommended for IVF with a husband’s sperm, since donor sperm is distinguished by excellent “health”, confirmed and proven by laboratory tests. In some cases, ICSI can also be performed with the donor's biomaterial, but this is relevant if the woman is single, and her oocytes, due to age or other reasons, have too dense shells that can not be punctured even by healthy spermatozoa.
Indications
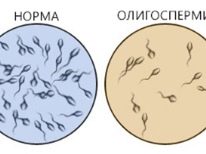
According to statistics, the share of IVF with ICSI accounts for approximately 65% of all extracorporal fertilization protocols. This means that intracytoplasmic sperm injection is in high demand. The need for a high-tech procedure does not always arise. It is indicated for poor spermogram, which could not be eliminated by conservative or surgical treatment. Here are just a few pathological conditions in which IVF + ICSI are shown for a pair:
- The total number of spermatozoa in the ejaculate is reduced to a critical point (oligozoospermia), or they are absent due to retrograde ejaculation, or ejaculation does not occur at all.
- The mobility of the male sex cells is perceptibly impaired (asthenozoospermia) - in the ejaculate, immobile and sedentary spermatozoids prevail, as well as sperm with irregular trajectory of movement, impaired coordination.
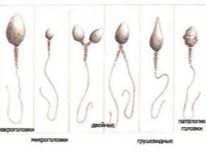
- Teratozoospermia is a condition in which morphologically modified sex cells mutants dominate in the ejaculate (two heads for one sperm, two tails or no tail, various modifications of the male sex cell structures.
- The presence of antisperm antibodies in semen.
- Idiopathic infertility, the causes of which after a thorough medical examination could not be identified.
- Low quality of oocytes caused by the natural aging of oocytes (in women older than 40 years), or having other causes (hormonal, congenital, effects of external negative effects, etc.). With some changes, the membranes of the oocyte become impermeable to spermatozoa.
- Failed IVF protocols for 2 or more cycles, if the quality of the germ cells of a man and a woman as a whole meets the standards.
It should be noted that ICSI makes it possible to become parents even in the most difficult situations, when no other methods and methods will help. Even if ejaculation does not occur, or there is not a single live sperm cell in the semen, doctors always have the practical opportunity to perform surgical collection of germ cells, for example, to do a testicular biopsy.
It will be enough to get only a few normal cells (whereas there are tens of millions in the ejaculate!) For ICSI to be successful.
How is it done?
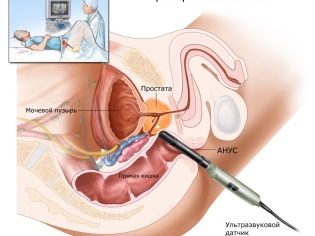
IKSI - surprisingly "delicate" work. It is absolutely impossible to inject a small sperm cell into the cytoplasmic space of an oocyte using a normal injection needle, the cells will be damaged and the embryo will not be obtained. For ICSI use hydraulic or electric micromanipulators. They are highly accurate. The whole process takes place under powerful microscopes.
In order to "work" with such fine material as human cells, special tools are needed - microneedles and micro-suckers. These tools are attached to the manipulators. And then the work of the embryologist doctor resembles a fantastic film - he makes movements with his own hands and the manipulator repeats his movements through the joysticks, but only on a microscopic scale.
For fertilization, it is important that the sperm DNA set is not altered. Therefore, in other parts of the sperm, in fact, there is no need. At the first stage, the embryologist selects the most healthy and morphologically normal spermatozoon and places it on the working surface under microscopes. Further, the micro needle needle interrupts the sperm tail. The cell becomes stationary - it is easier to work with it further.
In the tail with ICSI, there is no need, because the cage does not need to swim, aim, move. The most valuable - DNA, is in the sperm head.
Sperm left without a tail retracts into the micropipette needle. Microprice is retained egg. The sucker is on the left, the microneedle with the sperm inside is injected opposite - on the right. After puncture of the oocyte envelope, the contents of the pipette microneedle are inserted into the cytoplasmic fluid of the egg.
The question whether the egg can suffer from a puncture can be answered in the affirmative. But the probability of injury to the oocyte, according to available medical statistics, does not exceed 1%. In other cases, a rather elastic on the nature of the egg shell quickly tightened at the puncture site and inside it begins the most important processes of fusion of the genetic material of the future mother and the future father.
The egg cell is cleaned, placed in a special nutrient solution, where it will be in the next few days. Embryologists will cultivate the embryo if fertilization takes place before the moment when it is decided to transfer it to the uterine cavity of the woman.
Steps of the procedure step by step
ICSI does not exist as a separate program, it is part of the IVF protocol. Therefore, the main stages of IVF + ICSI are almost the same as with conventional IVF, in the protocol of which there is no need for intracytoplasmic injection of spermatozoa. If you are recommended IVF with ICSI, the procedure will proceed in several stages.
Training
At the preparatory stage, both partners or women (if fertilization is planned to be carried out with donor sperm), a detailed medical examination should be performed and a large list of tests should be submitted. The standard list for a woman includes general urine and blood tests, blood tests for HIV, syphilis, infectious viral hepatitis B and C, for TORCH infections, for hormones, for antisperm antibodies.
Be sure to undergo a gynecological examination, in which the order of the Ministry of Health of Russia includes ultrasound of the pelvic organs and mammary glands (women over 39 years old - mammography), colposcopy, hysteroscopy, determination of patency of the fallopian tubes, and vaginal smear tests on bacteria, microflora and infections.
The main analysis for men is spermogram. It should be done at least twice three months before IVF. With a bad spermogram, treatment to improve the quality of germ cells is shown, for which vitamin and mineral preparations are used, as well as dietary supplements that improve the spermatogenesis process.
In addition to the spermogram, on which the reproductive physician will rely in drawing up an individual IVF protocol, a man should undergo chest x-rays, blood tests, both for general and for HIV, syphilis and sexually transmitted diseases, as well as a smear from urethra
Collection of all necessary tests usually takes 2-3 months.This time the couple should be used sensibly - stop smoking and stop taking alcoholic beverages, start eating right, enriching the diet with meat, fish, cottage cheese and other dairy and dairy products, vegetables and fruits. Couple should go in for sports, but avoid excessive physical exertion.
It is not necessary to visit the bath, sauna. Especially this prohibition applies to men, who, on the eve of donating sperm for IVF for three months, should not be exposed to any heat from the scrotum. Overheating of the gonads located in it can significantly worsen the ejaculate indices at a crucial moment.
Protocol entry and stimulation
With the analyzes and the conclusion of the therapist that the woman is admitted to the IVF protocol, you should contact the fertility specialist 14-15 days before the next menstruation. On the first visit to the clinic, the couple will sign the necessary documents and will be informed of the type of protocol chosen by the doctor. If a long protocol is chosen, then before the onset of menstruation a woman may be prescribed hormonal drugs that suppress ovarian function, cause a condition resembling menopause. After 2-3 weeks, the woman is prescribed other hormones that stimulate the rapid maturation of the follicles in the ovaries.
With a short protocol, they do without first suppressing the work of the female genital glands. But the stage of taking hormones after menstruation (on the 5-6th day of the cycle) is necessarily present.
During the entire stage, a woman often goes to the ultrasound and donates blood for hormones. This allows the doctor to assess the growth rate of the follicles and prevent the inadequate response of the ovaries to hormonal stimulation - it may be insufficient or excessive. With insufficient, you can not get the right number of mature eggs for ICSI, and with excess, you can develop overstimulation syndrome, which in itself is very dangerous for women's health.
As soon as the follicles (at least three) reach sizes from 16 to 20 mm, HCG is administered to the woman. This hormone allows the eggs inside the follicles to ripen in an accelerated mode for 36-37 hours, after which it is possible to carry out the puncture of the ovaries.
Getting eggs and sperm
Sperm for the ICSI procedure is obtained in the traditional way - by masturbation. If it is permissible for a man to take the material at home and take it to the laboratory no later than 40 minutes before taking the analysis, then you need to take the sperm for IVF in the clinic immediately on the day when fertilization is planned.
On this day, the couple comes to the clinic together - the man goes to a separate room to collect the ejaculate, which is immediately delivered to the laboratory. If masturbation does not help (the man has no erection, the lower part of the body is paralyzed, there is no ejaculate, or retrograde ejaculation occurs), the procedure for collecting germ cells is performed under anesthesia by means of testicular biopsy or sperm extraction from epididymis.
If the procedure is carried out with the use of donor sperm, it is delivered from a cryobank, slowly defrosted in advance, and a study of the indicators of spermatozoa after cryopreservation is carried out.
In the laboratory, the biological material of a man undergoes primary cleaning, release from seminal fluid. Among the remaining concentrated sperm, only the best cells are isolated by microscopic examination, they are placed in a nutrient medium.
A woman is given a puncture of the ovaries to get eggs. The procedure is performed under general anesthesia, which is administered intravenously. Using a long, thin needle, an ultrasound-guided aspiration method makes a puncture through the vagina, withdraws the needle to the mature follicles and draws fluid from them together with the oocytes.
The patient remains in the clinic for a few more hours to get out of the anesthesia. Doctors observe her condition.From the day of the puncture, she is prescribed progesterone drugs that will help prepare the endometrium for implantation of embryos.
The resulting eggs are sent to the same embryology laboratory. They are freed from follicular fluid, washed, counted and the quality of the material is evaluated. The best and most viable eggs are allowed for fertilization.
Fertilization and transference
After the physician, with the help of a micromanipulator, transfers the selected sperm cells into the eggs, the observation period begins. If everything went well, after about 16 hours, the first changes are recorded at the microscopic level, and after a day the embryologist can tell exactly how many embryos were obtained.
Embryo cultivation lasts from 2 to 6 days - it depends on the protocol and individual recommendations. Then it is decided to transfer the embryo to the uterus of the woman. This procedure is fast, it does not give the patient any discomfort. A thin catheter in the uterine cavity will be poured a small amount of nutrient medium with a predetermined number of embryos.
On the one hand, a larger number of embryos increases the likelihood of pregnancy, but on the other hand, it creates risks of multiple pregnancies, and not every couple agrees to triplets or twins. Bioethics recommends that doctors choose the optimal number of embryos and convince their patients not to exceed it - in Russia there are 2-3 embryos.
The resection (removal of “extra” embryos after implantation) creates moral problems for many couples, and most world religions regard it as an abortion.
After the transfer, it is recommended to limit the motor activity. A woman is given a sick leave, and she can, with a clear conscience, spend several days in bed.
The wait lasts 14 days after the transfer, then the woman can do a blood test for hCG to find out if the pregnancy has occurred. A week later, you can do the first ultrasound to confirm and assess the condition of the uterus, ovaries and embryos.
Efficiency
The effectiveness of in vitro fertilization using ICSI in the protocol increases the likelihood of pregnancy. If conventional IVF ends in pregnancy only in 35-45% of cases, the success rate after intracytoplasmic sperm injection is somewhat higher - at the level of 50-55%.
Embryos after ICSI develop more successfully, because the sperm for fertilization is used without exaggeration selective. In 85% of successful pregnancies, a woman bears a perfectly healthy child. Unfortunately, the percentage of unsuccessful completion of pregnancy and complications during gestation after ICSI does not differ from the same indicator after usual IVF - 20% of pregnant women lose their babies in the early stages for various reasons - miscarriage, undeveloped pregnancy, ectopic pregnancy.
Future parents should know that ICSI does not guarantee the complete absence of congenital abnormalities in the fetus, because, unlike natural fertilization, which occurs several hours after ovulation, with ICSI, there is no natural selection.
With the natural conception, the spermatozoa are “screened out” at every stage of the passage of the genital tract, when trying to break through the membrane of the eggs. During ICSI there is no such selection, and therefore the probability of having a baby with pathologies still exists.
Many physicians and scientists are convinced that a child conceived by ICSI is more likely to inherit the diseases of the parents, which did not allow them to conceive a baby. If nature has not provided for a couple to multiply, then so it protects humanity from the birth of sick individuals. The method itself has nothing to do with it. This is just an attempt of people to “deceive” nature, to make it change its decision.
That is why a couple before ICSI, it is advisable to visit a geneticist, to make tests for compatibility and karyotyping.
If the doctor has data on hereditary diseases, he will also recommend preimplantation diagnostics after embryo cultivation - to make "screenings" of embryos that have inherited the ailment, and only healthy embryos can be planted in the uterus.
Advantages and disadvantages
Preparing for IVF with ICSI is identical to the usual preparation for in vitro fertilization, the couple will not have to do anything special, and this is the first plus. The undoubted advantage of the method can be considered an increased probability of a successful pregnancy. But a minus after all is that the probability of a little above 50-55% again does not guarantee the couple that they can become future parents in the current protocol.
The advantages include advanced features that gives the method pairs. These are women’s age (over 40 and even 45 years old if necessary), the ability to perform in vitro fertilization with HIV in a man without the risk of infection for an unborn child and a number of other situations from which it is difficult to find a reasonable way out using other methods.
The obvious disadvantage is the cost of the procedure, it is very high. If you can’t get pregnant the first time, the couple’s money will not be returned, and the next protocol will have to be paid again at full cost.
Moreover, sometimes this method cannot be used at all - a number of somatic and mental diseases, tumors, inflammatory diseases and developmental defects or post-traumatic changes in the area of the uterus and ovaries are contraindicated. Contraindications from the man does not exist.
Price
ICSI in the protocol leads to an inevitable and rather noticeable rise in the cost of IVF. The cost affects the selected region, a particular medical institution. On average, the cost due to the need to inject sperm into the cytoplasmic fluid of the oocyte increases by 50-125 thousand rubles.
If we consider that the average price of IVF in Russia in 2018 is 140-250 thousand rubles, it is easy to calculate the minimum and maximum cost of the same procedure, but with ICSI - 190-370 thousand rubles.
Do not believe the tempting promotional offers of clinics, which indicate on the Internet prices for ICSI and IMSI (selection of the best sperm) within 15 thousand rubles. This is obviously an advertising move, because in this case the incomplete cost is indicated. After adding the cost of drugs, reagents and nutrient media, the puncture payment amount will increase to the average Russian values.
The price is high, there is no guarantee of success - this is what stops many couples from trying to conceive a baby by this method. There is good news for them - now ICSI is included in the program of state support for IVF. You can get a federal or regional quota for the procedure and make it free of charge under the OMS policy. True, the amount of the quota is 141 thousand rubles in 2018. It may not cover the full cost of the protocol. In this case, the difference will have to pay extra.
Reviews
Positive feedback on ICSI among the majority of women who choose to share their own experiences with others in the thematic forums prevail. Many, even after several unsuccessful IVF attempts, managed to conceive the babies from the first time after the protocol with fertilization using the ICSI method.
However, one cannot ignore other reviews in which women describe their two, three or more unsuccessful ICSI attempts. There are even single reviews of fetal pathologies identified as a result of screening during pregnancy, which women tend to “write off” on the ICSI method, because the quality of spermatozoa, even the best of the choices the embryologist has, leaves much to be desired.
Women who do not want to experience severe hormonal stress, especially after several unsuccessful stimulated IVF protocols, often agree to ICSI in the natural cycle.The probability of success without the use of hormones is several times lower, because you can only get 1 egg (in the rarest case, two). And it does not guarantee that both will be suitable for the procedure, will be fertilized and transferred to the uterus.
Most often, women who are lucky and have a pregnancy after ICSI come claim that they were given two embryos - one was fertilized in a Petri dish using the usual IVF method, and the second was fertilized by ICSI to increase the chances of a successful onset of the long-awaited pregnancy.
If doctors recommend ICSI, experienced women should carefully choose a clinic and a specific doctor. Be sure to read all the available information about the specialist, with reviews of his patients.
If you can contact them personally, be sure to do it and chat. This will help to better prepare yourself mentally for the upcoming procedure and with the right attitude to go to the doctor for your future happiness.
How the ICSI procedure goes, see the next video.