How does the follicles puncture in IVF and how to prepare for the procedure?
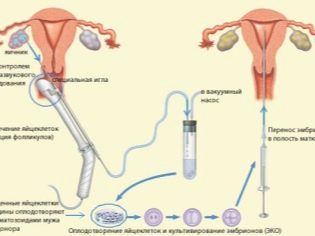
Puncture of mature follicles in IVF is an important step in the protocol on which the further treatment of infertility depends. How is this procedure and how to properly prepare for it, we will describe in this article.
What it is?
Every month a woman of reproductive age in one of the ovaries matures a follicle (sometimes two). After the monthly runs out, the process of ripening of this vesicle on the gonad begins. Under the influence of hormones, several follicles grow, but only one (rarely two) is destined to become dominant. It is from him on the day of ovulation will come out mature and ready for a meeting with the sperm cell egg.
During in vitro fertilization, there is not enough one egg, because the probability of conception and successful development of the embryo, and then the probability of implantation, the higher, the more eggs were obtained at the stage of preparation of the sex glands. A woman who is going to become a mother through the method of IVF, takes hormones. Follicle-stimulating hormones in the first phase of the menstrual cycle suggest that not one or two follicles will grow in the ovaries. Their growth is constantly monitored using ultrasound, and as soon as at least three follicles reach sizes from 16 to 22 mm according to ultrasound scanning, they inject the hCG preparation.
The injection of this hormone acts quickly and decisively. For 32-36 hours, it causes the operative maturation of the eggs. After that, the oocytes are required to be removed from the female body in order to proceed to the most important stage - laboratory fertilization. Oocytes can be obtained only in one way - by puncturing the follicles.
This procedure has the status of minimally invasive surgical intervention, it requires prior preparation and proper conduct by medical personnel.
How is it done?
Manipulation takes place in a small operating room. On the appointed day (exactly 34-36 hours after the introduction of the ovulation trigger), the woman arrives at the clinic, but this should be done in advance, at least half an hour to forty minutes before the appointed time. The doctor will do an ultrasound again to make a final count of mature follicles. Before puncture, they should be of sufficient size (about 18-22 mm).
Also, a woman is offered to solve an important question - what to do with the remaining eggs, if you plan to get a lot of them. In this case, she can agree to cryopreservation of her own germ cells, so that later, if she wants, she can use them for IVF, she can also donate them to the cryobank as donor (provided that the donor requirements for health, age and other parameters are met ).
Among other things, a woman can abandon them in favor of science, then scientists will receive the biomaterial to conduct various studies and tests.
Before the puncture, the woman measures blood pressure, pulse, and escorts her to the operating room. All manipulations are carried out on the bed of Rakhmanov. One day, if IVF is successful, exactly the same, you may have to give birth to your baby. A woman changes clothes in sterile clothes and shoe covers.
The anesthesiologist starts working with the patient first. Puncture of follicles is a painful procedure, and therefore in Russia it is not customary to do it without anesthesia.In some European countries, they try to carry out manipulation without the introduction of strong anesthetics, since a number of physicians believe that such drugs adversely affect the condition of the woman, complicate pregnancy and gestation in the future.
Russian gynecologists and fertility specialists are more humane, they do not want to deliver pronounced pain, moreover, they will be much calmer if the woman remains motionless during the delicate and delicate manipulation, which cannot be guaranteed if you do not give her anesthesia.
You can choose from general anesthesia with the use of a facial mask or intravenous administration of drugs that will cause a deep medication sleep with the absence of any sensitivity.
Some women who have read on the Internet about the "miracles of IVF in the United States or Israel", ask not to make them anesthesia. In this case, they are warned about pain. Local anesthesia during ovarian puncture does not exist. If the patient is determined to give up anesthesia, she will be given an anesthetic pill or be given an intramuscular injection in half an hour before the procedure. An important condition is that the follicles must be well accessible (this is determined on an ultrasound scan) and their number must be small.
If there are many follicles and access to them is difficult, the absence of anesthesia is out of the question. Particularly insisting on his absence may be denied a puncture. This requires medical ethics.
After the woman falls asleep, the most important thing begins. The most common method for obtaining oocytes from stimulated ovaries is transvaginal. When it is punctured in the vaginal fornix, they gain access to the ovaries through it. There is a second way to take eggs for fertilization - laparoscopic. It is used only when a woman's ovaries are located abnormally.
A special long puncture cannula is used transvaginally to collect eggs. It is inserted into the vaginal fornix, into its posterior wall, and then carefully advanced by the doctor in the direction of the follicles. Each of them sequentially, in turn, pierce and aspirate (suck) its contents through a needle into a special container. The follicular fluid together with the ovules is sent to the laboratory in a polymeric vessel, where embryologists are already waiting.
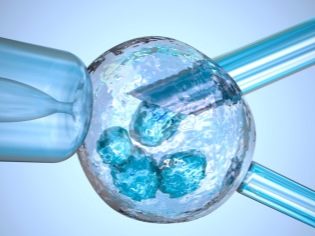
These specialists will conduct a primary inspection of oocytes, wash them from follicular fluid and other impurities and provide the eggs with a “warm meeting” with the sperm of the husband or donor in the Petri dish or ICSI method, in which the selected sperm is inserted into the cytoplasmic fluid of the oocyte directly under the membrane.
Puncture needles, which are used to collect oocytes, have a special coating, which should prevent traumatization of the female ovaries, and the internal coating of the needles does not allow “crippling” the eggs themselves as they pass through the follicular fluid in the system. All the details of what is happening, doctors in real time are watching on the monitor of the ultrasonic device. At the end of the puncture needle there is a small air bubble, which serves as a “beacon”, which “detects” the ultrasonic sensor.
Doctors often receive prophylactic manipulations after receiving follicular fluid, which should prevent overstimulation syndrome, which can occur as a consequence of aggressive hormone therapy (especially often after Dekapeptil and Clomiphene). For this, the same needle, without removing it, is advanced along all the follicles that have grown up, but insufficient for fertilization. A needle doctor removes them as unnecessary.
Approximately 60% of physicians do not find such prophylaxis useful, since it increases the likelihood of infection or trauma. They are limited to only puncture for the production of oocytes, without affecting other follicles.
In any case, they try to pierce the vaginal fornix only once, and all subsequent manipulations are performed through one puncture, changing the angle and depth of penetration of the puncture needle. It is not always possible to get an egg, the reason for the lack of opportunity may be the inaccessibility of one or another follicle for puncture. If access can be dangerous from the point of view of the development of a female gland injury with a puncture needle, such follicles do not pierce. The whole process described lasts no more than 15-20 minutes.
A woman is transferred to the ward, where she gradually wakes up, “departs” from anesthesia and gains clarity of thinking. The monitoring is carried out by the attending physician. Being in the ward is taken from 2 to 4 hours - it depends on the individual response of the fair sex to anesthesia. As soon as the doctor finds that the woman’s condition is quite stable, he will give her recommendations on how to proceed with the further regimen and let her go home for a few days, until the time comes to transfer the embryos into the uterine cavity.
Puncture preparation
Preparation begins long before the IVF protocol. In order to get better eggs during the course of treatment and to increase the chances of maturing several full-fledged oocytes, a woman is recommended to have a protein diet, sufficient amount of vitamins, as well as the obligatory presence of sufficient and caloric nutrition. It is necessary to exclude excessive, exhausting physical exertion, whether it is physical work in the country or trips to the gym.
A woman is not recommended to bathe in the bath and take hot baths, limiting herself to a warm shower. Also, do not take any medications, if it is not allowed and not prescribed by a doctor - medicines can adversely affect the quality of germ cells. You should quit smoking in advance, alcohol intake is not allowed.
Since most surgical procedures are usually prescribed for morning or lunchtime, women should not be eaten from the evening of the previous day. In the morning do not need to drink fluids. If the procedure is performed on an empty stomach, the chances of normal tolerance of anesthesia are higher. Sleep on the eve of the operation should be complete, at least 8-9 hours, you should eliminate stress, anxiety.
With a woman in the clinic you need to take only your passport and a list of appointments, which was filed with the entry into the protocol. Do not wear contact lenses, earrings, rings, chains, bracelets. Hair should be carefully collected. Makeup will be clearly redundant.
Feeling after the procedure
After puncture of the follicles, the woman may feel light dizziness, drowsiness. Valid are not abundant pinkish discharge from the genital tract. They are associated with mechanical damage to the vaginal fornix during a puncture and pass quickly enough - usually the state normalizes during the day and the discharge stops.
It is also quite natural to consider a slight temperature rise to subfebrile values (37.0 - 37.8 degrees). After puncture, the woman is given a single large dose of a broad-spectrum antibiotic, which should prevent possible inflammatory processes after the intervention.
Also, usually from the first day after the puncture (that is, on the day of the procedure), progesterone drugs are started. Usually, Duphaston or Utrogestan is prescribed in individual dosages.
A woman is strongly advised to behave after a puncture as carefully as possible - to eliminate stress, stress, sexual relations. On the first day it is better to lie down and relax, sleep, read a book or watch a movie. On the second day you can do household chores, but without fanaticism. A high-calorie protein diet is recommended.It is necessary to reduce the amount of salt consumed, as well as to abandon products that can lead to more intensive gas formation in the intestines (peas, beans, black bread, kvass, yeast pastries, baking, cabbage, oranges).
A woman is recommended to drink plenty of water.
If after a puncture lower abdomen hurts, it is quite normal. The intensity of the pain syndrome depends on the number of punctured follicles and on the method of obtaining oocytes. With transvaginal pain management, the pain most often subsides the next day. If the fence was performed by means of laparoscopy, the pain may be present for up to 3-4 days, while often there is a feeling that the stomach “swelled”, and constipation may occur.
Among the most unusual complaints about the state of health after the collection of oocytes, according to women, it is possible to note paroxysmal headaches, jumps in blood pressure. But these symptoms can be attributed not to the very puncture of the follicles, but more to the consequences of the action of anesthesia. In some cases, patients after manipulation disrupted nighttime sleep. Usually in a few days everything is restored.
On the question of what can be taken from the medicine after a puncture, the attending physician will answer best. Usually, but-Shpa is recommended for abdominal pain, but it is also recommended to take it with a headache. When constipation, you can use rectal candles "bisacodil" or microclysters. Low-grade fever after a puncture does not need a medical reduction. It is important not to forget to take in time the hormonal agents prescribed by the doctor, the preparation of the endometrium of the uterus for the upcoming embryo implantation depends on it.
The recovery period after a puncture lasts usually 2-3 days. Just a day after the puncture, a woman can find out how many embryos have turned out, another day she can tell how many of them develop and grow normally. Usually, two-day, three-day, or five-day embryos are transplanted into the uterine cavity. This will be decided by the attending physician.
Probability of complications
At the present level of development of medicine, complications after collecting oocytes are extremely rare. But every woman who has to undergo such a procedure needs to know about them. First of all, it is necessary in order to notice the symptoms of complications in time and promptly seek medical help. A completely human factor can have negative consequences - an insufficiently experienced doctor can injure a blood vessel, in which outflow of blood can occur in the abdominal cavity. It is also theoretically possible injuries of the ovaries, the development of turbovarial space, ovarian abscess, ovarian torsion.
No matter how terrible it may sound, the statistics are rather optimistic - such complications do not occur more often than in 0.5-1% of all cases of puncture of the follicles.
The most common complication is the development of ovarian hyperstimulation syndrome. But this is rather a consequence of the preceding hormonal stimulation, rather than the process of puncture of the follicles itself. When overstimulation of the ovaries increases in size, this is accompanied by a rather strong pain in the abdomen and lower back. Such a complication, according to statistics, occurs in 2.5-3% of cases.
The true origin of the syndrome has not been established, but there is an assumption that it starts the injection of hCG, and it still seems the most likely. Due to the shift in the balance of hormones in the body of a woman, the permeability of the vascular walls increases, as a result not only an increase in the ovaries can occur, but also an accumulation of blood in the abdominal cavity.
The most frequently affected are women under the age of 35 years old, with a deficiency of body weight, with polycystic ovaries, as well as women with allergies, women with elevated levels of estradiol in the blood.In a slight degree, hyperstimulation syndrome is observed in all those who undergo hormonal preparation for collecting oocytes in the IVF protocol, but in most cases everything goes by itself and does not need to be corrected. Medium and severe forms of the syndrome are considered dangerous for the health and life of women.
Thus, the appearance of small edema, weight gain, abdominal distension and pulling weak pain in the lower abdomen, speak of a mild form. In more serious situations, vomiting, nausea, diarrhea, increasing swelling and thickening of the abdominal wall appear. The amount of urine excreted by the kidneys decreases, "flies before eyes" can appear, hands and external genital organs swell dramatically.
A woman should be more attentive to her well-being. When the temperature rises above 38.0 degrees, with increased pain, the appearance of severe edema and vomiting, an ambulance should be called. A woman must be taken to a hospital where she will be provided with necessary medical care.
In this case, embryo transfer can be delayed until a more suitable moment. Embryos are cryopreserved until the next protocol.
The transfer can also be canceled if, after the puncture, the woman has exacerbated chronic diseases, signs of viral infection (ARVI, flu, etc.), signs of infection, and fever.
Monthly after puncture follicles without transfer usually come within 3-5 days after discontinuation of progesterone drugs. If there is no transfer, the woman is immediately recommended to stop taking Utrozhestan or Duphaston. The menstruation itself can be more painful than usual.
Reviews
According to numerous reviews of women in thematic forums, there is no need to be afraid of puncture. Everything passes quickly and is not felt by a woman. Unpleasant sensations after the procedure can be fully endured, they are not painful.
Many women note that at the preparatory stage, doctors numbered 15-18 follicles, and during the puncture they managed to get only 2-3 eggs. Most of the follicles are empty, and some are cysts.
About anesthesia mostly positive reviews. Women call him gentle and claim that they transferred him well, within an hour they felt quite cheerful, and after two hours they calmly went home. After the laparoscopic collection of eggs, the recovery process after anesthesia is longer and feels much worse, according to women.
To make it all go more successfully, popular rumor recommends that a woman wear red panties, striped socks and a red T-shirt. It is not very clear how tissue color can affect the success of puncture, but experienced women try to follow this rule rigorously and recommend that beginner ECO shnitsam, those who entered into their first in vitro fertilization protocol.
The puncture and the hormonal stimulation preceding it take a lot of energy. In order for a woman to be more relaxed before the main stage - the embryonic stage, doctors often recommend sedatives. According to reviews, the most appointed is the tableted motherwort, as well as "Persen».
The greatest part of the negative reviews about the procedure was left by women who puncture the follicles without anesthesia. Some refused it for personal convictions. Others performed the procedure in foreign clinics, where they try not to give anesthesia. The procedure is described as rather unpleasant, painful. Of course, women's motivation is “iron” - they want to become mothers, but it is not necessary to endure pain.
Infrequently, but it can happen that the rupture of the follicles occurs before the puncture is made. In 10% of cases, this is detected during the puncture. In 50% of cases, doctors, according to reviews, manage to “catch” oocytes in the ampullary part of the fallopian tube, where they go after ovulation. This is not reflected in the subsequent fertilization and viability of embryos.Just the puncture itself turns into a kind of quest for the doctor. Sometimes it is not possible to “catch” them and the protocol is closed until the next time.
From the following video you will learn how the puncture is performed, which doctors and medical staff are at the puncture of the follicles, how much time you need to spend in the hospital, and whether you need time to recover.