How do IVF? The main stages and features of the procedure
In vitro fertilization gives infertile couples a real chance to become parents. At times, this is the only way out and the pair have particular tender expectations for the procedure. How is IVF, what are its main stages, and what will be the steps step by step, we will tell in this article.
What it is?
IVF exists in the world medical practice for over 40 years. For the first time a child conceived in a test tube was born in 1978 in Great Britain. This girl is now 40 years old and she herself is a happy mother. In Russia, ancillary methodology has been widely adopted since 2012, when the IVF program received government support in the fight to improve demographic indicators. In total, more than 4 million children born through IVF live on the planet. Every year more than 100 thousand IVF are done in Russia.
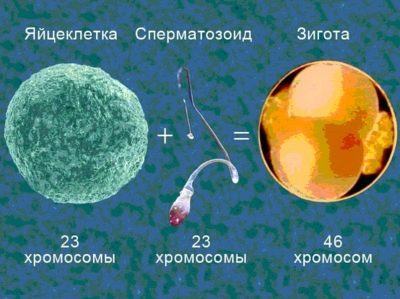
In vitro fertilization implies conception outside the maternal organism. Genital cells of men and women are carefully selected. Fertilized eggs are also given close attention. Only the best embryos are transferred to the uterus of the woman for further bearing.
The effectiveness of IVF in our country is estimated at an average of 35-45%. The success of the procedure is influenced by many factors: the woman’s age, the health of her and her partner, whose biomaterial is used to fertilize female oocytes, the correctness of the IVF protocol choice by the doctor, as well as the individual response of the female body to the medicines that she will have to take. However, no one can ever give guarantees that a pregnancy will be 100% complete, even if both partners are young and relatively healthy.
In Vitro Fertilization is recommended if the treatment of infertility of a man or a woman by other means did not bring the desired positive result.
For IVF, women who have no ovaries, impassable fallopian tubes or none, women and men with severe endocrine and idiopathic (undetected) forms of infertility are sent to IVF with a high risk of transmitting the genetic pathologies of mother or father to offspring.
For IVF in Russia quotas are provided, then the procedure is carried out under the policy of compulsory medical insurance. You can also contact reproductologists for a fee.
Kinds
Depending on the reason why a couple cannot conceive a child naturally, Doctors can offer various types of in vitro fertilization, which differ in process and stages.
- If a woman has preserved ovarian function, the eggs mature and have a satisfactory quality, and the age of the planning pregnancy is no higher than 45 years, then it is usually performed. stimulated IVF protocol. It can be long and short (the difference is in the number of days of taking hormonal drugs). Stimulated IVF has a higher impact on the statistics of occurring pregnancies, because it allows you to get a larger number of oocytes and even keep them frozen for the next attempt, if the first one fails.
- If a woman has contraindications to the use of hormones, but ovarian function is preserved, doctors can suggest IVF in the natural cycle. Such fertilization is carried out without medical support, it is more natural for the female body, but, alas, the effectiveness of the procedure is much lower, because only 1 can be obtained in such a cycle, and in rare cases 2 eggs, no more. Accordingly, the chances of pregnancy will be several times less.
- If a woman has lost ovarian function, does not produce her own eggs, or their quality is unsuitable for fertilization, it can be carried out IVF using a donor egg. Donor fertilization will be offered in the case of total male infertility, but with the use of donor sperm. If a woman has no uterus or diseases and defects of the main reproductive organ are not subject to correction and interfere with pregnancy, fertilized eggs can be implanted by a surrogate mother, who endures and gives birth to a long-awaited baby.
- IVF with frozen donor eggs, own oocytes, sperm and embryos, carries the name cryoprotocol. Such IVF can be both stimulated and natural.
- Auxiliary technologies may require such jewelery accuracy that fertilization will be performed using only one egg and one spermatozoon, while the male germ cell will help to penetrate the egg cell, inserting it under the shell of the oocyte with a thin hollow needle. This IVF will be called ECO + ICSI. The technique is recommended in particularly difficult cases.
Preparatory stage
Preparations for in vitro fertilization begin several months before the cycle in which an attempt to become pregnant is planned. First, men and women who want to become parents, will have to gradually pass all the tests and pass all the necessary examinations so that the couple will be allowed to enter the IVF protocol.
The woman will have a full range of gynecological examinations, ultrasound of the pelvic organs, vaginal smears for infections and microflora, as well as instrumental and surgical methods of examination, such as colposcopy, hysteroscopy. She will need to follow all the doctor's instructions for blood tests for hormones (different hormones are determined at different times on the days of the menstrual cycle). In addition, it will be necessary to pass tests for HIV status and syphilis, viral hepatitis B and C, TORCH infections, as well as sexually transmitted diseases.
A man will need to make spermogram, which will show the state of his ejaculate, vitality and motility of sperm and their morphological features, as well as blood tests for HIV, syphilis, genital infections and a smear from the urethra. Both partners do a chest X-ray of the chest organs and undergo general urine and blood tests. Couples, in which a woman is over 35 years old or a man over 40 years old, undergo genetic tests for compatibility, karyotyping and receive a separate admission of a geneticist.
If any inflammatory diseases, infections, or pathologies are identified, the treatment is first carried out, and only then the date of entry into the protocol is set. This first, preparatory stage may take several months. In preparation for IVF, spouses are advised to maintain a healthy lifestyle, stop smoking and taking alcohol even in small doses, take vitamins and eat right.
You should not visit the bath and sauna, soak for a long time in a hot bath, wear tight and tight underwear, so as not to disturb the blood supply and thermoregulation of the pelvic organs.
If IVF is planned with its own oocytes and spermatozoa, it is at this stage that the pair are advised to take drugs to improve the quality of the eggs and spermatozoa.The regimen of medications and vitamins prescribed by the doctor, it usually fits into periods of up to 3 months.
A couple should carefully avoid viral and infectious diseases, because an increase in temperature during the flu or ARVI can postpone IVF for another couple of months, as it negatively affects the state of male and female reproductive health.
At the end of the training, the couple is invited to sign an agreement and a written consent to conduct IVF. It specifies all the nuances, including legal ones, as well as the couple undertakes to protect themselves during the entire month of the protocol, but only with barrier contraceptives - condoms.
Entering into the protocol
7-10 days before the beginning of the next menstruation in a woman, a couple should come to an appointment with the selected doctor in their chosen clinic to enter the IVF protocol. The protocol refers to one scheduling attempt and all actions necessary for it. In the IVF treatment cycle, only couples are introduced who have all the test results available, and have signed agreements and an agreement for the provision of medical services.
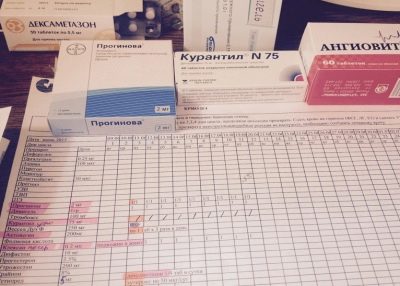
The woman is given a control ultrasound of the pelvic organs, if necessary, office hysteroscopy to assess the internal state of the uterus. After that, the woman is given an individual sheet of medical appointments. It contains detailed instructions and rules of life for the coming month. At each next appointment, a woman will have to come with this list of appointments.
On the day of entry into the protocol, the doctor determines the protocol’s features, indicates on the prescription list the names of the prescribed medications, their dosage, frequency of administration and duration of therapy, and also indicates when the woman should come for an appointment next time.
Each stage of IVF should be paid by the couple in advance - before the start date of the stage, if IVF is done not according to quota, but at the own expense of the family. If at one of the stages the doctor decides on the termination of the protocol due to advanced complications or an unfavorable prognosis, the money for the stages that have not yet been completed is returned in full without commission. Funds paid for already completed stages are non-refundable.
Ovarian stimulation
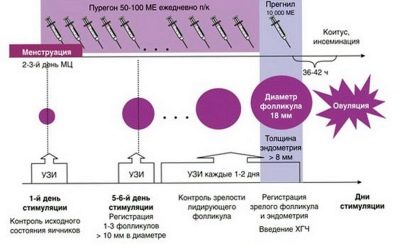
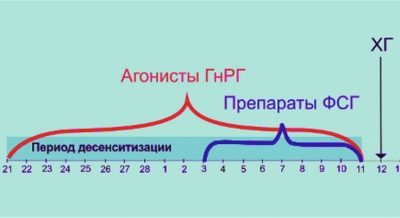
This stage begins either before the beginning of the month, or after their completion. It depends on the choice of the duration of the protocol. Most often, IVF in Russia is carried out using a long protocol. With it, a woman begins to receive hormonal drugs 10-14 days before the start of the next menstruation.
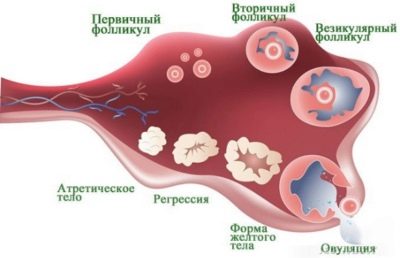
During this period, medications inhibit the activity of the ovaries, a state of "artificial menopause." This is a preparation for the main stimulation. At the end of the training, the doctor prescribes other hormones, the task of which is to stimulate the growth of follicles in the ovaries. The more follicles mature, the more eggs can be obtained at the next stage of treatment. A large number of oocytes increases the likelihood of successful fertilization and implantation.
In a normal menstrual cycle, a woman usually matures one egg, rarely two. Stimulation of superovulation by hormones allows you to get from 10 to 20 oocytes.
During stimulation, a woman will have to come to the reception several times - donate blood for hormone levels, monitor growing follicles by ultrasound. It is important that doctors "catch" the most optimal time for the collection of mature eggs. In addition, the ovarian response to stimulation is important. Control allows you to identify an insufficient response in time, and then the doctor increases the dose of hormones or changes the drug. It is also important to avoid an over-response - ovarian hyperstimulation syndrome.
With a short or ultrashort IVF protocol (and they are used less frequently), the woman begins to take hormones without first suppressing the work of the sex glands, after menstruation, and completes on the 10-13th day of the cycle.In this case, monitoring the growth of follicles is also mandatory. There is no need to pay for each ultrasound, usually 4-5 diagnostic procedures are already included in the cost of the stimulation stage. This amount is enough for high-quality ultrasound monitoring.
As soon as the doctor states that the follicles have matured, their diameter exceeds 18 mm, the total number of such follicles is at least three, he prescribes an injection of HCG. This hormone is administered once 36 hours before the collection of eggs, so that the oocytes are able to ripen in an accelerated manner. Immature oocytes are unsuitable for fertilization and cannot guarantee the conception of a healthy and full-fledged embryo.
At the stage of superovulation stimulation, a woman may notice a deterioration in well-being - dizziness, nausea, nagging pain in the lower abdomen and lumbar region, and slight swelling. In case of any deterioration of well-being, you must immediately inform your fertility specialist about them.
Egg and Sperm Collection
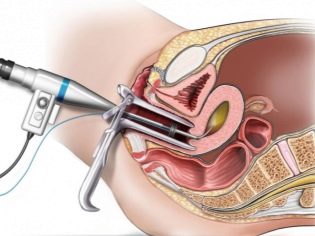
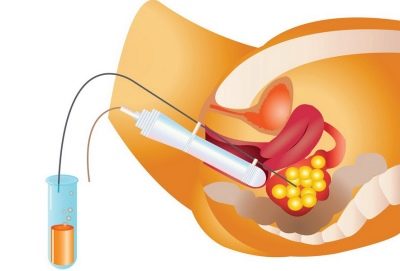
36 hours after the injection of hCG, a woman needs to go to the clinic to undergo the procedure for collecting eggs. This is done by puncture. The woman is located on the gynecological chair, a cannula is inserted into the ovaries through the back wall of the vagina, through which the doctor pulls out the contents of the stimulated follicles along with the eggs.
The procedure is painful, therefore it is performed using anesthesia. Usually, anesthesia is administered intravenously. The entire intake process is monitored by an ultrasonic sensor in real time. This allows you to carry out the procedure with maximum accuracy.
The resulting follicular fluid with the oocytes contained in it is placed in sterile containers and immediately sent to an embryology laboratory for the initial assessment of the quality of the eggs obtained. Manipulation lasts no more than a quarter of an hour. For three hours, the woman remains under the supervision of doctors after leaving anesthesia, after which, in the absence of complications, she is sent home.
10-12 hours before the puncture it is forbidden to take food; it is not recommended to drink liquid for 8 hours. On the eve of a puncture, a woman should not have sex. In the morning of the procedure, it is imperative to do an enema and clean the intestines. Do not apply makeup on the day of the fence, wear contact lenses. Chains, earrings and rings should also be left at home.
After the procedure, there may be minor pain in the lower abdomen and lower back, small blood-like discharge from the vagina, nausea, headache. These symptoms usually disappear in a day. A woman is recommended to take a single dose of antibiotic to prevent inflammation.
And from the day of puncture, she is prescribed drugs to maintain the function of the corpus luteum, which is formed at the site of the exposed follicles. Usually prescribed "Utrozhestan" or "Duphaston." These preparations also help the endometrium to increase its thickness, to become looser, so that the chances of successful implantation are higher.
By the time the puncture ends, the woman’s partner must have delivered a fresh portion of sperm, which will be used for subsequent fertilization. This is done by masturbation in a separate office of the clinic. Seminal fluid is also sent to the laboratory for examination. There are no recommendations for a man after sperm donation. He can lead a normal life.
If the amount of sperm is very small or because of the male factor of infertility, ejaculation does not occur at all, doctors can perform a surgical collection of sperm. The procedure is also carried out under general anesthesia, in 2-3 hours a man can leave the clinic.
A woman is recommended a quiet mode, good nutrition and the complete absence of stressful situations. If the temperature after puncture is higher than 38.0 degrees, the appearance of abundant discharge from the genitals, bloating of the abdomen, severe pain, pain during urination, you should call an ambulance. But the likelihood of such complications after puncture, if it was carried out correctly and in compliance with all requirements, is minimal - no more than 0.1-0.3%.
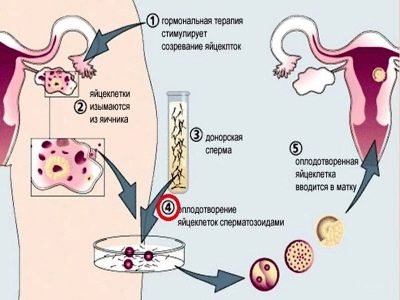
Fertilization
The mystery of the birth of new lives occurs in the laboratory. From the follicular fluid under a powerful microscope, oocytes suitable for fertilization are isolated, counted, and placed in a special incubator with a nutrient medium. There they are 4-5 hours, after which they add concentrated sperm to the incubators. To increase the chances of fertilization, they try to count in such a way that each egg cell has at least 45-50 thousand male germ cells.
If such a number of healthy and motile sperm is not detected in the ejaculate, ICSI can be performed - the introduction of selected reference spermatozoa under the egg membranes “pointwise” and purposefully. It is clear that ICSI significantly increases the cost of an in vitro fertilization protocol.
If the protocol uses frozen eggs and sperm, before they are combined in an incubator nutrient medium, a gentle defrost and careful microscopic screening of damaged and unsuitable cells is carried out. The effectiveness of cryoprotocols, contrary to popular belief, is no less than when using fresh germ cells, which were obtained a few hours ago.
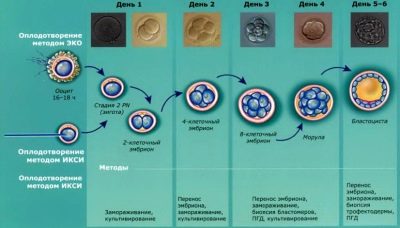
Signs that fertilization has taken place are observed in the ova already on the same day, which is commonly considered zero. The first changes at the microscopic level are observed approximately 16 hours after the joining of the oocytes and sperm. However, doctors will be able to accurately determine the number of successfully fertilized oocytes only in a day.
It is after 24 hours that the doctor will be able to answer the question of how many embryos are received. If fertilization did not take place at all, the pair will have to start all over again. If in advance at the stage of entry into the protocol, the possibility of ICSI should be discussed with the doctor, then it can be carried out in the current protocol.
Cultivation of embryos and their diagnosis
As soon as fertilization took place, the egg cell acquires a new status, now it is a zygote. This unicellular embryo already contains the maternal and paternal chromosomes, has a gender, it contains all the genetic information - how tall a person will be, what will be the color of his eyes, hair, what inherited diseases he will suffer.
On the second day after fertilization, which are now called the days of cultivation, the embryologist assesses how the zygote is broken up. The rate of this process and the quality of the resulting embryos are evaluated. Already at this stage, preimplantational diagnostics of the quality of embryos can be carried out in order to detect possible deviations in their development.
Only embryos that have undergone a qualitative assessment are allowed to be transferred into the uterus of the future mother. The transfer itself can be made on the second or fifth day of its existence. Most often, doctors prefer to observe the development of fertilized eggs to 5-6 days, when they become blastocysts. It is at this stage during the natural conception that the egg is descending into the uterine cavity, and in another day or two, implantation into the uterine wall occurs.
If a couple has been prescribed by geneticists regarding possible pathologies of the fetus, blastocyst embryos are examined for inheritance of the disease. If there is a risk of a disease linked to the sex chromosome, the embryos will be divided into boys and girls and only embryos recommended by the geneticist will be allowed to replant. In other cases, the sex of the embryos is not determined and it cannot be announced to parents before replanting.
In Russia, since 2012, a law has been in place to ban embryo discrimination on the basis of sex. It is impossible to “order” a child of a certain sex in our country without medical indications.At the end of the cultivation period, the doctor contacts the spouses and invites them to come to embryo transfer.
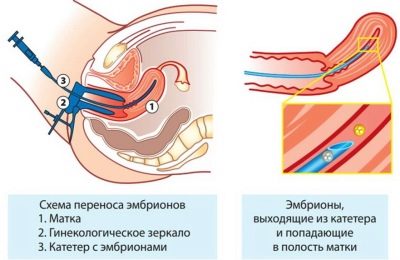
Embryo transfer
Five-day blastocyst embryos are more likely to implant, so when transferring the "five-day week" there is no need to plant a large number of embryos. Accordingly, the likelihood of multiple pregnancy is reduced. The transfer of “two-days” or “three-days” also has its pros and cons.
On the day of the transfer, a woman needs to arrive at the clinic in advance. It is not necessary to take a spouse with him, there is no need for him in his presence. But if he wants to support his beloved, doctors will not interfere. It is not necessary to come hungry, doctors usually allow a light breakfast, but drinking is not recommended so that a woman has no problems with a full bladder.
A pair at this stage needs to make the most important decision - how many embryos will be transferred to the uterus. They will be warned about the likelihood of multiple pregnancies (according to statistics, this happens in 60% of cases of IVF with a replanting of 2-3 embryos).
If there are many embryos, the spouses will have to decide the fate of the rest. They can be frozen and will be stored in a cryobank in case the couple wants more children, as well as in case of an unsuccessful current protocol, so that in the next protocol it is possible not to resort to hormonal stimulation, puncture, but simply carry out the transfer during the implantation window.
The pair can donate embryos as donor for other infertile couples, as well as transfer them to scientists for research. The spouses fix their decision by signing documents in which all the conditions of the fate of the embryos are agreed and agreed.
After that, the woman is placed in the gynecological chair, and the doctor introduces the required number of blastocysts into the uterine cavity through a thin catheter attached to a disposable syringe. The procedure is quite simple, painless and does not take much time.
About an hour a woman should be in a horizontal position and try not to move. After that, she is allowed to get dressed and after receiving the recommendations of the doctor with a detailed description of the lifestyle after replanting, she can go home.
Subsequent period
This period is the most painful in terms of expectation, in which a woman and her sexual partner are located. Uncertainty about whether or not implantation has taken place causes chronic stress in women. Woman shows the maximum rest. Therefore, after the transfer, she receives a sick-list.
At home, she was advised to lie more or follow the half-bedding regime, showing good sleep, normal nutrition, rich in vitamins and all the necessary minerals. Excitement, emotional upheavals should be excluded, because stress hormones prevent the development of your own sex hormones and reduce the chances of implantation. To maintain hormonal levels from the day of embryo transfer, the dose of Utrogestan or Duphaston is usually doubled.
It is necessary to take drugs in full accordance with the list of appointments in the indicated dosages without forgetting. Sometimes, the need to use these medications persists until 14-16 weeks of pregnancy, until the placenta begins to independently produce the hormones necessary for the preservation and maintenance of pregnancy.
A couple of days after the transfer, the woman may well return to her usual lifestyle, but we should exclude smoking and alcohol, as well as any excessive exercise, from carrying heavy packages from the supermarket to the refrigerator and ending with a visit to the gym. Take a hot bath is prohibited. On the first day after transplanting, it is not allowed to wash or swim at all. Then you should take a warm shower for hygienic purposes. Sexual relations with her husband at this stage are strictly contraindicated.
During this period, women may experience a scanty scanty discharge from the genital tract. This is not considered a pathology. Also, the appearance of a few drops of blood approximately three to five days after transplantation is not considered a pathological phenomenon — this may be implant bleeding, which suggests that the implantation of the embryo in the endometrium has taken place. If there is no such symptom, there is no need to despair - not every woman has implantable bleeding after the onset of pregnancy.
A doctor should be consulted if the discharge is increased, if there is cramping pain in the lower abdomen and in the lower back, if there are blood clots in the discharge, the temperature has risen. Neither the woman nor her doctor can affect the implantation process. The likelihood of a successful pregnancy is not increased by medicines, it is outside the competence of doctors. But following the recommendations will help a woman get rid of the feeling of guilt that many people experience after an unsuccessful IVF attempt.
Pregnancy diagnosis
Test strips for pregnancy after IVF should not be used, because a woman was given an injection of hCG for the maturation of eggs, and traces of chorionic gonadotropic hormone could remain in the body, therefore, a probability of a false positive result is high. On the 14th day after the infusion, it is necessary to analyze the quantitative content of hCG in the blood plasma. This analysis makes it possible with 100% probability to say that the pregnancy took place or did not take place.
If several embryos were implanted at once, the amount of hCG will proportionally exceed the average rate - 2 times, if a woman becomes pregnant with twins, 3 times - if triplets now live in her womb.
Lowered levels of hCG may be caused by late implantation. A woman is recommended to retake blood after two days. Before the analysis is not recommended to eat, take any medications, in addition to the prescribed by the attending physician.
Chorionic gonadotropin, on which the diagnosis is based, begins to be produced by the chorionic cells only after the implantation of the ovum. Its concentration, subject to adequate development of the embryo, doubles every 48 hours. If the embryo has taken root, and then rejected, the level of hCG by the 14th day after the transfer will also be significantly below the norm.
On day 21 after the transfer, that is, one week after a positive blood test for hCG, the woman is recommended to make the first confirmatory ultrasound in the same clinic where all previous stages were performed. The first ultrasound examination can be scheduled a little later - during the week from 21 to 28 days after the transfer.
Ultrasound research will allow not only to establish the fact of pregnancy, but also to determine its features - the number of fruits, the place of attachment of the ovum, its viability. Closer to 28 days after the transfer, the expectant mother can already hear the heartbeat of her baby or toddlers. It is important to exclude an ectopic pregnancy, missed abortion, the threat of miscarriage or miscarriage that has begun, as well as any other pathology.
31 days after the transfer, a second ultrasound study is conducted, which demonstrates how dynamically the embryo develops (or several embryos). At this point, obstetric gestational age will be 6-7 weeks, and a woman may well be registered in the antenatal clinic.
After a successful second ultrasound scan, an extract of the protocol is given on hands showing all stages, medications, dosages and features. There are included the results of laboratory tests of the future mother. With this extract, you should go to the gynecologist in the antenatal clinic for further pregnancy until delivery.
Next steps
With a positive result of the diagnosis of pregnancy, questions about further actions practically do not arise.A woman is registered, however, she again has to take all the tests and make examinations for entering into the exchange card of a pregnant woman and a woman in labor. The results of the surveys that she underwent before IVF will not work.
If the result of the blood test for hCG, unfortunately, turned out to be negative, this means that the pregnancy has not come, the progesterone drugs are canceled from that day, you no longer need to take them. After the end of the next menstruation, the woman must again contact the fertility specialist to examine and identify the causes of the absence of pregnancy. They make ultrasound, hysteroscopy again, donate blood for hormones and infections. If necessary, correct the protocol, change medications, dosages.
Sometimes it is quite productive to simply change the type of protocol - from long to short or ultrashort, from stimulated to natural or cryoprotocol. In general, the probability of success in the second protocol is always significantly higher than in the first. In addition, the couple has all the chances to unexpectedly become pregnant naturally: after the hormonal "push", which was given to the female body, about 25% of the pairs get to conceive the baby in a completely traditional way.
After the stimulated protocol, a break of 3 months is required. This time is necessary so that the woman's body can take a break from the hormonal load. After IVF in the natural cycle, you can plan the next protocol as early as next month. After an unfavorable termination of the pregnancy that occurred in the first protocol (miscarriage, missed abortion, ectopic pregnancy), a break of 5-6 months is necessary. After these periods, the woman may well plan with the doctor a new IVF protocol.
During the rest period, all measures should be taken to improve the quality of the germ cells of partners - take vitamins, eat well, keep a mobile and active lifestyle.
It is important for a woman to cope with negative emotions and disappointment after unsuccessful IVF as quickly as possible, because depression and feelings only reduce the likelihood of success in the next protocol.
Reviews
The most emotionally difficult period during the entire IVF protocol women call the latter - the waiting period for the result. During this period, the main thing is not to rush things and not to worry from scratch, and it is precisely this that often presents considerable complexity.
The most difficult from the point of view of well-being for women usually becomes the first stage - stimulation of the ovaries. In addition to a temporary deterioration and well-being, many complain that amid high doses of hormones, they significantly gained weight, and problems with hormonal acne began.
If the family does not have enough money, but really wants to become parents, they will have to be patient, because according to the law, IVF under IVF can be done once a year for free. The number of attempts is not regulated by law. Another question is that, according to women, not every clinic is taken for IVF by OMS, if a woman is over 35 years old, if she has poor tests or the probability of success of the procedure is low. If it is necessary to use a donor biomaterial, the couple will have to pay for it separately from its own pocket.
Also, women who have been through IVF for CHI emphasize that not all analyzes and surveys are compensated by the social insurance fund. Some, for example, semen is done only on a fee basis. As a result, the IVF protocol on the quota obtained is still quite expensive.
More information about the main stages of IVF will tell the fertility specialist in the next video.