Features of anesthesia during childbirth and after
Clinical recommendations of the Ministry of Health give women the right to demand pain relief for childbirth at any stage, because no one should tolerate unbearable pain. But anesthesia during childbirth is different, and its use may have its own characteristics.
Kinds
Anesthesia during childbirth is not considered something mandatory, unless it is a caesarean section. Childbirth is a natural process, and therefore need and need for anesthesia is far from occurring in every case. But a woman who is preparing to become a mother should know that, according to the law, doctors should provide her with anesthetic methods if she asks for it. This is provided in the clinical protocol for obstetrics, which is the main guide to action for obstetricians.
The pain threshold for different women is different. One is more enduring contractions, the other suffers and is experiencing severe stress even with not the most intense labor contractions.
There are several types of anesthesia that can be used in the generic process:
- general anesthesia;
- spinal anesthesia;
- epidural anesthesia;
- analgesia by intravenous administration of light painkillers.
General anesthesia
General anesthesia for natural childbirth is not applicable, since it implies a complete lack of consciousness and muscle activity. The woman is deeply asleep, and therefore immune to pain in general. This method is used during cesarean section. Recently, general anesthesia has been used less frequently, epidural anesthesia has come to the first place. Usually, during surgical labor, general anesthesia is done endotracheal. Prepare for it in advance if the operation is planned, or carry out on an emergency, if the operation is emergency.
Before plunging the woman in deep sleep, premedication is administered - atropine is injected so that the heart does not stop in a state of anesthesia. Then potent analgesics are administered intravenously and the expectant mother falls asleep. She no longer feels like the surgeon inserts a tube into the trachea and connects it to a ventilator. The anesthesiologist has the opportunity at any time to add a dose of narcotic substances, if suddenly the operation is delayed. As the work of the surgeons is completed, the doctor reduces the dosages of the drugs, and gradually the woman wakes up. The smoother the reduction in dosage, the smoother the awakening will be. The tube from the trachea is removed before the woman comes to himself.
This type of anesthesia is considered conditionally safe for the mother and fetus, although the effect on the fetus does take place: the baby is more sluggish after birth, but gradually it goes away. Psychologically, this type of anesthesia is considered more convenient, because a woman is not forced to be present during her own surgery, as is the case with epidural anesthesia. The drugs are stored in the blood of the puerperal 3-4 days after delivery, but in doses that can not affect her consciousness..
General anesthesia has no contraindications. But with a newborn, the newly-made mother does not occur immediately, but only after a few hours.
Epidural and spinal
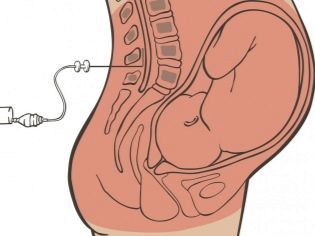
This method refers to the methods of regional anesthesia and today is considered the most common. It can also be used to relieve contractions and to perform a cesarean section. In this case, analgesics are administered not intravenously, but epidurally, that is, into the epidural space of the spine through a thin catheter, which the anesthesiologist introduces.
The drugs block the nerve impulses in the lower body. Depending on which goal is worth, they are administered either more or less analgesics. With caesarean section, the sensitivity of the entire lower body is removed; during childbirth, the dosage of drugs is lower so that the woman still feels her legs., but did not feel unbearable pain in the fights.
The woman sits or lies on her side, the doctor finds the desired point of injection and slowly inserts a catheter with a shot into the spine, and then injects it with medicine. The catheter remains in the spine, if necessary, the doctor can add painkillers. The effect comes after 5 minutes.
The woman remains fully conscious, can talk with the obstetric team, understands everything she is told and is able to fulfill the requirements of the doctor. With a caesarean with such anesthesia, a woman can see her child immediately after he is removed from the womb.
The probability of complications from such anesthesia does not exceed 1 case per 50,000 births. These include insufficient anesthesia, injuries of the spinal canal and nerve endings, hematoma formation, spinal fluid leakage, which is fraught with subsequent severe headaches.
The consequences for a child with such anesthesia are less pronounced, but still they are also present. Some lethargy in a child, lethargy is observed within a few hours.. According to reviews, pain sensitivity is often preserved, although it is rather dull.
There are contraindications to this type of anesthesia - women who have bleeding disorders, spinal injuries, obesity, rashes on the skin of the back in the place where the puncture is planned to be performed, do not have it, where a woman has low blood pressure or bleeding occurs or there is a reason to assume hypoxia in the fetus .
Spinal or spinal anesthesia is carried out as an epidural, but the introduction is deeper - not in the epidural space of the spine, but in the subarachnoid. Due to this, the effect of anesthesia is stronger, and not always spinal anesthesia is indicated during natural childbirth.
Selection
Theoretically, any woman in labor can choose anesthesia, but there are situations when only doctors make a choice. In natural childbirth, the choice is small - either light analgesia or epidural anesthesia, if there are no contraindications. In preparation for cesarean section, a woman can express her wishes by choosing between general and epidural anesthesia. She signs an informed consent in which it is indicated that she is warned about the consequences, complications, techniques of anesthesia.
If the pregnant woman refuses epidural anesthesia, she is given general anesthesia.not having contraindications. Do not ask for the views of the woman in childbirth when the child needs to be rescued as soon as possible - with a tight cord entanglement, for example, or if it is necessary to remove the uterus after cesarean.
In natural childbirth, a woman also has every right to both ask for anesthesia and refuse it, even if doctors insist. This is a personal matter, but in this case, the consequences of refusal will be explained to her.
With complications
Rapid labor, a violation of the coordination of uterine tone during labor, generic weakness - these conditions require a special approach to anesthesia.
With prolonged contractions that are irregular and do not lead to a significant opening of the cervix within 12 hours, the woman is exhausted, tired, and the fetus suffers. In order not to bring the woman to the extreme, doctors can decide on the introduction of sedatives and analgesics intramuscularly. For this, diazepam and baralgin are most commonly used. After removing such contractions, proceed to emergency measures aimed at the urgent maturation of the cervix.
If the labor activity is uncoordinated, it is dangerous placental abruption, the development of severe bleeding, uterine rupture and the death of the baby. The incompetent and excessive anesthesia that was performed to a woman earlier, as well as drug stimulation of labor activity, often leads to such a condition. In this case, the woman is administered drugs that will plunge into a short (3-4 hours) sleep for rest and recuperation.
The weakness of the generic forces is manifested by insufficient activity of contractions, weak opening of the neck. The woman is very tired, she also shows a pharmacological dream. For this, 20% oxybutyrate or ketamine intramuscularly is administered intravenously in dosages that are perfectly safe for both women and children.
Women with preeclampsia and hypertension may be given tranquilizers and antispasmodics.
Alternative pain relief during childbirth
Non-drug anesthesia of labor is considered the most preferable. It is applied first of all, and if there is no action, only then it is reasonable to consider the issue of medical anesthesia. Such methods include, in particular, method of psychoprophylactic preparation. Its essence is to eliminate stress and fear of labor. This is done by doctors of women's clinics, specialists of courses for expectant mothers. Stress leads to the production of adrenaline and cortisone hormones in high dosages. In response, the muscles tighten, including the muscles of the uterus and cervix. Disclosure is difficult, and the pain increases in the majority solely for psychogenic reasons.
It is important to tune in the right way to childbirth, to perceive them as work, work that will be richly rewarded.
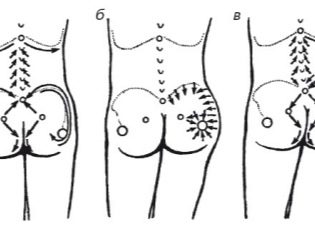
Massage of the sacral area helps to reduce pain during contractions, which a woman can spend on her own or seek help from a partner if the birth is a partnership.
Effective self-pain relief occurs with proper breathing exercises.. Deep and slow breaths, smooth and long exhalations stimulate the production of serotonin - the hormone of joy, which not only has a beneficial effect not on the nervous system and psyche of the woman, but also has a certain anesthetic effect.
There is a whole list of postures in which it is easier and easier to endure the birth pains. Nobody in a maternity hospital makes a woman lie on a bed. Until the attempts began, she can take any poses, move as she likes, if, of course, there are no complications in which the horizontal position is shown.
Negative effects on the child non-drug methods do not have.
Afterbirth application
After a natural birth, anesthesia is usually not necessary. The exceptions are situations when a woman had an episiotomy (surgical dissection of the perineum to facilitate the birth of the fetus) or tears. In the first days after such childbirth, light painkillers intramuscularly can be recommended, focusing on the intensity of the pain. Pills are not recommended painkillers.
After cesarean section, anesthesia is mandatory during the day., then - as a woman. When breastfeeding, the use of painkillers in the first days after childbirth is not contraindicated. When a woman is discharged from the hospital, she may also have situations in which anesthetic is required.When the lactation is already established and the child is fully breastfed without formula, you should always consult with your doctor to find a drug that penetrates to breast milk to a lesser extent and enters the child.
The name of the means and the dosage should be prescribed only by a doctor, self-treatment for HB is absolutely contraindicated.
If there is a need for anesthesia after childbirth (emergency surgery, cleaning, etc.), then anesthesia is performed, but after it for 3-4 days breastfeeding is not recommended, while residual doses of drugs for anesthesia remain in the blood.
Reviews
The use of epidural anesthesia in childbirth women is ambiguous. Some are sure that she practically did not help them, others argue that the birth was easier because of anesthesia. Almost everyone claims that pain relief has some consequences - Women for several months after giving birth suffered from headaches and complained of pain in the back.
Those who had a caesarean section also have different opinions. Some support general anesthesia, others are satisfied with epidural. As for doctors, they indicate that each type of anesthesia has its advantages and disadvantages. Only non-drug alternative anesthesia does not have disadvantages.
Learn more about the methods of pain relief childbirth learn in the video below.