Contagious mollusk in children
Children's skin is so sensitive to everything around that a variety of rashes on her parents sometimes do not even surprise. However, there are skin diseases that many moms and dads have not even heard about. However, these diseases often affect children. About what is molluscum contagiosum and how to treat such a disease in a child, we will tell in this article.
What it is
Molluscum contagiosum is a skin disease of viral origin. When it affects mainly the skin, but sometimes suffer and mucous membranes. Characteristic rashes resembling the shells of mollusks on the skin are caused by a virus belonging to the smallpox group, but not smallpox as such. It is considered close to smallpox.
This virus is capable of infecting only humans; animals do not get sick of it and do not tolerate it. And most often the cunning agent attacks precisely children from birth to ten years. There are four types of this virus. The first and second, indicated by the corresponding sequence numbers after the name of the pathogen MCV, are usually transmitted sexually. This is a disease of adults.
But MCV-3 and MCV-4 are varieties of molluscum contagiosum virus, which most often affect children. The virus is spread by contact. Quite often they are infected through common toys, household items, dishes and linens. However, the agent may well survive in the aquatic environment, and therefore often attacks children attending the common pool.
Another local distribution path is self-infection. A child who has several elements of skin rashes, combing them, spreading the infection to neighboring healthy skin. So increase the scale of the lesion. Molluscum contagiosum is contagious, so a child who has been diagnosed with such an infectious disease should not attend kindergarten or school. Parents should always inform the caregiver and the class teacher of the disease.
In the children's team, heightened security measures are being introduced, and the skin of other children is carefully examined by medical personnel.
The incubation period is from 3 weeks to six months. The first signs of the disease, therefore, can only be detected after a considerable time. In newborns, the incubation period lasts less, and dermatological disease manifests itself faster - after 2-3 weeks. The risk of infection for infants is represented by parents who are sick with molluscum contagiosum, relatives and family friends who come to visit, and there is also a chance to receive the virus in the so-called vertical way - from mother to child during pregnancy.
Despite its frightening name, this virus is not dangerous, it does not threaten the life of a child. In most cases, it does not even require specific treatment. However, situations are different, and sometimes the need for therapy still appears.
Causes of disease
A child who is confronted with a poxvirus (molluscum contagiosum virus) does not have to become infected with it. Most often, the disease occurs in children with insufficiently formed immunity.
At risk:
- children with HIV infection and other diseases associated with a deficiency of the immune system;
- children attending large children's groups;
- often ill children who are characterized by some kind of immune "apathy";
- children with a history of dermatological and allergic diseases;
- children who neglect hygiene;
- children aged six months, when babies are no longer under the protection of maternal innate immunity.
For quite a long time, particles of the contagious mollusk virus can live in the environment, in dust, in the air. But they become active only after penetration into the body fluid. For them, such is the substance that is filled with skin rashes. And because the risk of infection exists in the case of the child getting wounds, scratches, abrasions.
Even after infection, the virus may not manifest for a long time, and the first rash usually coincides with other factors that indirectly “accelerate” the appearance of mollusks on the skin.
These factors include:
- severe stress or prolonged stress that the child is experiencing;
- acute viral or bacterial disease;
- negative factors from the outside - inhalation and skin contact with toxins, carcinogens, allergens;
- food or drug poisoning.
Until the end, the mechanisms and causes of the action of the posquirus have not yet been studied, and in many issues concerning this pathogen, physicians and scientists do not agree on one thing, but almost all specialists agree on one thing - a person with strong, hardened immunity is ten times less likely to become contagious. clam, even by direct contact with it. But to explain why the virus can affect both the skin and be characterized by subcutaneous nodules, science is not yet able.
Symptoms and signs
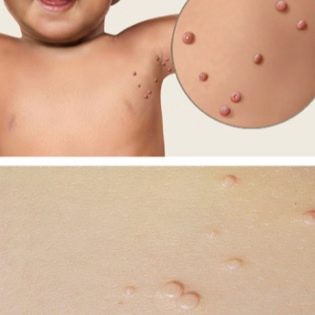
The main and practically the only symptom of the disease is a skin rash. She has the character of individual papules. Each has a rounded or oval shape. Their size can be as small as possible — from 1 mm in diameter, or as large as several centimeters.
At the initial stage, papules have a typical skin color, and almost do not stand out. But pretty quickly, the rash becomes pink with an orange tinge, acquiring a mother-of-pearl tip. If you press on the top, it may seem thick white cheesy discharge, as from some acne. Sometimes the papules in appearance resemble the cells of red blood cells, "pancakes" of a dense consistency. In the center of each disc is a small depression, resembling the navel of a person.
At the very beginning of the disease papules have small sizes. Quite quickly, they expand and can reach a diameter of 7-10 millimeters. If the mollusks reach values of more than 2 centimeters, doctors talk about the gigantic form of the disease.
Quite rarely papules are located on a certain elevation above the skin, on a small movable "leg". Then the disease is called pedicle.
With numerous small papules, the molluscum contagiosum is called a miliary. The most common form is when a child has 1-2 papules, sometimes their number reaches ten. In adults, the viruses MCV-1 and MCV-2 are most commonly seen on the thighs and genitals. In children, the “geography” of the third and fourth type of molluscum contagiosum virus is more extensive. Most often the first papules appear on the skin of the face, on the body, on the arms and on the legs. The characteristic pink hemispheric formations are often located exclusively locally - only on the nose, on the head, on the neck, in the eyebrows and on the chin.
If a child begins to comb, rub or squeeze papules, the infection will quickly spread further - on the chest, on the back, on the stomach. At the early stage, the papules are quite hard and dense. Gradually, they soften and become more friable. Pain rash does not cause. However, many children complain that papules are itchy, itchy.
The disease does not always need treatment, since the molluscum contagiosum passes on its own.True, it takes a lot of time - from several months to several years. Most often, the recovery process takes a period of six months to a year.
Traces on the skin papules after recovery do not leave. Scars and cavities as effects are more characteristic of the close relative of the poxvirus, the smallpox virus. However, the large size of papules and extensive lesions, coupled with a weakened child’s immunity, may be good reasons for therapeutic measures.
Diagnostics
Any pediatrician is able to recognize a contagious mollusk, as they say, in the face. Diagnosis even during the initial visual inspection does not cause significant difficulties. By the appearance of papules, by opening one of the papules by the manual method, it is possible to establish the correct diagnosis.
Sometimes, in order to ascertain his assumption, the doctor will take the contents of one papule for laboratory analysis. In this white, gritty mass, ovary epithelial cells are usually found in the laboratory undergone significant degenerative effects. Inside these cells, there are protoplasmic inclusions, which are called Lipschütz mollusks.
If no microscopic examination of the contents of the papules is found, the doctor will review the diagnosis and examine the child for warts, acne, scabies, keratoacanthomas.
Other additional analyzes and studies for molluscum contagiosum are not required. After confirming the diagnosis, the child will be sent for a consultation with a pediatric dermatologist, who will be able to answer the main question - whether you need to treat the baby or better wait until the disease passes by itself.
Treatment
As already mentioned, the contagious mollusk is able to pass on its own, however, it will take quite a long time to wait. Doctors do not agree to this if the child has immunodeficiency (HIV and other pathologies of the immune system), if he has a serious concomitant infectious disease, and also if the papules are located on the eyelids or genitals. The parents sometimes disagree on the many months' waiting, especially if the papules of the molluscum contagiosum are located in a prominent place - on the face, on the nose, on the eyes, on the hands of the child.
In all these cases, they are offered a variety of ways to treat the disease. To be more precise, there is no way to treat the clam, you can only eliminate cosmetic defects - the papules themselves. However, until the child is completely self-healing, the appearance of new elements is quite realistic under adverse circumstances. Immunity to the virus is produced, but it happens very slowly. If during an acute respiratory viral infection the body is enough 3-5 days to take control of the situation "in its hands" and suppress the virus, then with a contagious mollusk the period of development of immunity is calculated for months and even years.
If the doctor claims that there is no need to treat the child, and the parents want to rid the baby of papules, then no one will interfere with them, and the doctor will advise one of the treatment options.
Curettage
This method should not be carried out at home on their own, it is desirable to undergo the procedure under sterile conditions of the clinic. The temptation to do everything at home with their own hands is great, because the procedure is quite simple. But the consequences of home treatment can be sad - this is primarily an infection.
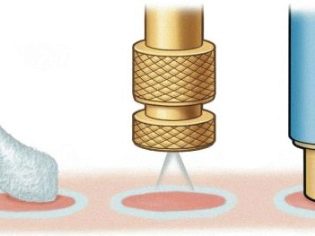
The method involves removing the head with tweezers and scraping the papules with a curette or a special tool - Folkman's spoon. When the cavity of the papule becomes clean, it is burned with iodine. Sometimes the doctor is limited to only thin tweezers, with small rashes this is quite enough.
This method has more minuses than pluses. Judge for yourself - the procedure is quite painful and unpleasant. The child, even with the use of an external spray with an analgesic effect ("Lidocaine, For example), it will be quite difficult to sustain curettage to the end.This method is categorically not suitable for removal of papules located on the face, especially in the eye area, because after curettage there is a risk of minor local bleeding, and also there are often depressed deep scars on the skin.
Parents who, in numerous reviews on the Internet, advise not to spend money on cosmetic procedures, and spend it all at home, are doubly at risk - the possibility of infecting the child with pathogenic bacteria is added to the possibility of skin defects.
Cryodestruction
Papula molluscum contagiosa is quite possible to remove liquid nitrogen or dry ice. This procedure is offered by almost any clinic. Papules are destroyed under the influence of liquid nitrogen rather quickly, the procedure is painless, does not require anesthesia. However, according to patients, still delivers some quite tolerable discomfort.
The substance is held on the area affected by molluscum contagiosum for no more than 20 seconds, after which the surface is treated with an antiseptic. In this case, the manipulation can be carried out both in hardware and tampon (manual) way. The place affected by dry ice or liquid nitrogen temporarily demonstrates all the classic signs of a thermal lesion - it turns white, edema appears around the cautery site, which can last for about 3-4 hours.
Then a small bubble forms around the frozen papules, which it is absolutely impossible to pierce so as not to infect the child. The frostbitten papule itself is rejected in about a month and a half. This method is not considered the most successful in order to get rid of the contagious mollusk on the face and all exposed parts of the body. Bubbles that occur under the influence of cold, often leave marks on the skin in the form of small scars, even after recovery.
In addition, in childhood there is often an allergic reaction to the cold. To avoid such consequences, it is advisable to pass a test in advance on such allergy and begin cryodestruction only when the child is allowed this intervention.
Electrocoagulation
This method is based on cauterization of the papules of a contagious mollusk with high-frequency alternating current. Under the influence of current, the skin surface and papule heat up, the mollusk dies, a small crust forms in its place, which itself leaves after a week and a half. The procedure is carried out with a special device electrocoagulator. Pre-skin anesthetize. After cauterization, the former papules are treated with iodine or another antiseptic. The result is evaluated in a week. The disadvantage of the method is that not all papules can die. Sometimes the procedure has to be repeated.
Laser treatment
To date, this method is considered the safest and most effective. In the clinic, papules are acted upon by a pulsed laser, pre-anesthetized the skin with an anesthetic in the form of a cream. The affected skin area under the laser beam warms up to 150-155 degrees. At this temperature, the virus dies, and the contents of the papules are evaporated. The high temperature also completely disinfects the site of exposure, which eliminates infection by bacteria and fungi.
The effect does not have to wait long. Already after the first session of laser therapy, about 90% of molluscum contagiosum papules die. Most often, one session is enough that completely defeat the disease. After the laser exposure, reddened spots remain in place of the semicircular spherical papules, which usually pass fairly quickly.
Therapy does not leave scars, scars, cavities and other defects, which is why the method is considered most suitable for removing clams from the skin of a child if they are located on the face, near the eyes, on the nose, on the chin.
After such an impact, it is impossible to wet the places affected by the laser beams for three days.The child should not attend the pool, bath, shower, sauna. After three days you can return to normal life. The minus of laser therapy is that it is contraindicated in newborns and children with other skin diseases of microbial, fungal or allergic origin.
Medications
For the treatment of molluscum contagiosum, the method of chemical cauterization of papules is used. It should be understood that the rash on the skin with this disease are of viral origin, and therefore they are completely insensitive to alcohol-based antiseptics and to "Zelenka". All drying means can also be dangerous, since papules should not be dried.
Among other medicines use:
- Of antiseptics often used "Fukortsin". It allows you to stop the spread of infection, especially if the child is constantly combing, injuring and tearing papules. Lotion "Molustin", Although it is not a drug, but belongs to the category of cosmetic preparations, leads to the destruction of infected cells and quite effectively eliminates papules, but it can only be used for children from 3 years.
- Good help treating ointment containing tretinoin. It "Vesanoid», «Lokatsid". These drugs are not prohibited to use in childhood, but the manufacturers do not have sufficient and convincing results of clinical studies on children. Before use, be sure to consult a doctor. If he approves, the ointment is applied on papules twice a day for at least 5-6 hours, after which the affected skin is washed with warm water and soap. Procedures continue until the complete disappearance of the last papule.
- Non-protein poison cantharidin, which underlies such a well-known drug, as "Spanish fly", Is also quite often used to treat molluscum contagiosum. However, with this tool you need to be extremely careful, because this poison can cause severe poisoning. For children under 7 years old, you should always consult a doctor.
- Cream "Imiquimod”, Which is often advised to use in molluscum contagiosum, does not have antiviral activity, and it is undesirable to use it for children under 18 years of age. It is better to give preference to oxolinic ointment. This drug is applied to papules in a thick layer 2-3 times a day.
- Quite often, doctors prescribe for the treatment of molluscum contagiosum "Isoprinosine"And"Acyclovir". "Izoprinozin" is an antiviral agent, an immunomodulator. Appointed to children over 3 years old in pills in dosages directly dependent on the weight of the child. "Acyclovir" - antiviral ointment, which is designed to combat herpes viral infection of various types. Acyclovir does not show great activity in relation to the contagious mollusk, but it objectively accelerates the healing time of papules at the final stage after mechanical stress or cauterization.
- It should be noted that taking antiviral drugs in no way affects the duration of the disease. They do not accelerate recovery, and even more so do not save the child from the papules of the mollusk. All doctors are well aware of this, but continue to prescribe their small patients with such a diagnosis of suppositories. "Viferon", Homeopathic"Anaferon"And"Otsilokotsinium". This is often done in order to create the appearance of treatment, because a doctor who will say that these papules should not be treated at all, parents may not understand.
Taking antibiotics for molluscum contagiosum is impractical, since antimicrobial agents generally have no effect on the virus. In rare cases, the doctor may recommend an antibiotic ointment, but only if the child has a bacterial infection, and some papules, previously injured, began to fester and become inflamed.
Traditional methods of treatment are based on smearing papules with garlic juice, tincture of calendula, extract infusion and bird cherry juice. However, experts do not recommend self-treatment, as papules are easily damaged, and in the absence of sterility, the risk of infection will increase many times. Recovery is the period when the last mollusk on the skin has disappeared in the child.
Immunity is not lifelong, and after some time re-infection may occur.
Prevention
The best prevention of molluscum contagiosum is by following the rules of hygiene. It is important that a child from an early age learn to use only his personal towel, brush, slippers. Change of underwear should occur daily, and bedding is changed once a week. If a child goes to the pool and goes swimming or goes to the public bath with his parents, It is important that after each such visit he take a shower and change into clean clothes.
If there are several children in a family, then the person infected with a molluscum contagious is transferred to a somewhat isolated state. It is clear that it is impossible to limit the child in communication for a whole year, until all papules disappear from him. But it is quite enough to prevent close physical contact, as well as sharing the same toys, dishes, towels and linens. For a patient, all this must be his own.
One of the main points in the prevention of molluscum contagiosum is to strengthen children's immunity. From a very early age you need to harden the child, to ensure long walks in the fresh air. In older age, sports are welcome. Food should be balanced and saturated with all the necessary vitamins. In periods of high incidence of viral respiratory infections, it is better to refrain from visiting public places with a child with large crowds of people, from traveling by public transport at rush hour, from visiting clinics and hospitals unless absolutely necessary. Immunity is promoted by preventive vaccinations, which are provided for by the National Vaccination Calendar.
You should not abandon them, because vaccines are also training for immunity, which will not allow the child to become infected with dangerous ailments, as well as reduce the overall seasonal incidence of ARVI.
See the next video for what is contagious mollusk and how to fight it.