What to do if a child has been bitten by a tick?
A little tick can make a person a big problem. Especially its bite is dangerous for children whose immunity is imperfect and is in the process of formation. The consequences may be the least pleasant. In this material we will tell how to find a tick on a child’s body and what to do next.
Who is he?
Ticks people used to be considered insects. But they really are not.
A tick is an animal; this is the definition given to it by medical reference books and manuals on biology. Moreover, this animal has much in common with spiders, and therefore attributed to a subclass of arthropods arachnid.
To imagine the diversity of these blood-sucking parasites, it is enough to know that more than 45 thousand species of ticks are known to science. Not all of them, it should be noted, are carriers of infections, but those that do not pose such a danger may well cause local skin irritation and inflammation, especially on tender and vulnerable children's skin.
Common types of ticks are real cunning hunters. They can watch for a very long time sacrifice, hiding on the leaves of trees, on bushes. After waiting, the tick clings to the skin, takes root and begins to feed on human blood. Feel the bite is not immediately due to the fact that the animal is accompanied by local anesthesia - secretes with saliva special substances that suppress nervous sensitivity.
In most Russian regions, the dangerous epidemic season begins in April and ends only in the fall. The most dangerous time is from mid-April to the end of July. A tick can attack a child on a walk in the woods, in a forest-park zone within the city, in a public garden, in a country house, in children's camp.
Danger and consequences
A tick bite is dangerous in that even short contact with this animal can result in infection. Diseases with which a tick can “reward” its donor are quite dangerous:
Tick-borne encephalitis
The damage to the central nervous system is a special virus, the carriers of which are about 5-6 of the ticks. The chance of being infected by biting such animals in an adult varies from 2 to 5%, and in children from 5 to 7%.
The disease is severe with all signs of brain damage, with high fever and fever. Fatalities are not excluded.
Tick-borne borreliosis
An infection that occurs when a bite of ixodic ticks, which are borrelia carriers. These spirochetes cause extensive neurological or heart diseases in the child, as well as arthritis and atrophic dermatitis.
In some regions, the number of borrelia carrier mites reaches 90%, which means that virtually every bite represents a real risk of infection.
Tick fever
They are also called spotty fevers. This is a group of febrile states accompanied by a rash, discoloration of the skin, muscle pain, lymphadenitis. Complications can be quite serious.
Ticks can also cause fever, occurring through the hemorrhagic type with kidney damage, as well as some other types of territorial focal febrile conditions.
The most dangerous are co-infectionswhen the baby is infected from the blood-sucking parasite is not one specific type of virus or bacteria, but several at once in the complex.Such a probability also exists, and it cannot be ignored.
About 15% of ticks in the population are just carriers of a whole "bunch" of infections.
Symptoms and signs
Not to miss the signs of a tick bite will help attentive attitude to the child. After a walk in the park or in the forest, a trip to nature, it is advisable to carefully examine the body of the child.
Ticks most often choose places like ear space, neck, chest. It is possible to detect the parasite on the head, in the hairy part of it the animal feels protected.
You should carefully examine whether there are traces of a bite on the body, on the arms and legs, in the groin and in the armpits.
The bite site always looks like erythema (redness) with a diameter of about 0.7-1.0 cm. If the parasite does not spontaneously fall off after the meal (the males often do this, whereas the females prefer to stay with the donor as long as possible), then in the middle of the spot will be himself. On the surface always remains the body of the tick, head submerged under the skin.
Redness is nothing more than a local allergic reaction to tick saliva. The form of erythema is always round or oval. When you click on the redness of the child does not feel pain.
If the body of the tick is no longer there, and the parents doubt whether the red spot is a bite trace, then wait a few hours.
Usually, 5-6 hours after tick bites develop chills, weakness, drowsiness. A little later, the temperature may rise to 37.0 - 37.5 degrees, regional lymph nodes may slightly increase. All these are signs of a bite, the child must be shown to the doctor.
If the parasite itself is detected, then it is easy to recognize the bite. It is much more difficult to provide the child with the correct emergency care.
First aid
The algorithm of parental actions in detecting a tick should be as follows:
- carefully remove the animal;
- to treat the wound - bite mark by any means with strong antiseptic properties;
- put the parasite in a container, for example, in a can, tightly close it and take it to the territorial department of Rospotrebnadzor, where it is examined by laboratory;
- On the 11th day, take the child to the clinic, where it will be possible to donate blood for analysis, which will determine whether an infection has occurred;
- caution should be given to karapazu antibiotics to prevent possible diseases;
- if the tick attack has occurred far from hospitals, laboratories and civilization in general, then it is worth giving the child a dose of antibiotic and an antiviral agent as an emergency aid;
- to conduct a close observation of the child for 30 days - in case of deterioration, to hospitalize the child.
How to get the parasite
It is necessary to remove ticks from the child’s body decisively and as quickly as possible. The longer the tick remains there, the greater the risk of infection. It should be noted that this is not an easy task. The arthropod parasite holds very tight, and it is impossible to just take it out.
Leaving part of the tick in the wound can not be, it can cause severe inflammation.
Until recently it was thought that mites should be spread with turpentine, kerosene or oil. However, I would like to warn parents against such actions.
Deprived of the opportunity to get oxygen under the oil layer, the tick becomes desperately aggressive. In an effort to survive, he throws a maximum of his saliva into the child’s blood. (its reserves, by the way, are quite large), so the risk of infection with Borreliosis or encephalitis increases tenfold.
To strangle the tick in terms of the safety of the offspring is a bad idea.
For removal you can use:
- durable thread;
- tweezers;
- a special set of "Antiklesh" (you can buy in a pharmacy or medical equipment stores)
- own hands.
If none of the above is present, then you should not take the tick with unprotected fingers. If the tick's body is damaged, its intestinal contents may be in the bloodstream, and this is very dangerous.Therefore, for manipulation it is best to use rubber medical gloves, a bandage or a piece of cloth, for example, a handkerchief.
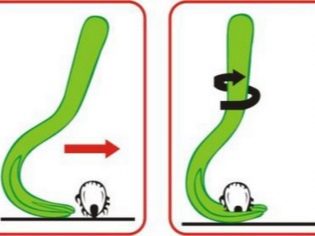
Removal with tweezers is done like this:
- the capture of a tick as close as possible to its head immersed in the skin of a child;
- turn it clockwise 6-7 times;
- output of the parasite by the movement itself.
Fetching is carried out in this way:
- on a strong thread an eyelet with a diameter of about 2 centimeters is made;
- the loop attaches to the tick as close to the head as possible;
- tighten the “stranglehold” and start twisting the thread clockwise or counterclockwise;
- as soon as the thread is completely twisted, the parasite is pulled out with a slight movement towards itself.
Removing the parasite with your fingers looks like this:
- protected hands tick capture as close to his head;
- turn the tick 6-7 times clockwise;
- take out the parasite.
Wound treatment
Means suitable for treating a wound after the expulsion of an animal:
- brilliant green solution ("Zelenka");
- iodine;
- alcohol;
- "Chlorhexidine";
- hydrogen peroxide.
Apply compresses and bandages to the bite site after treatment is not necessary.
Drive the tick itself to the laboratory only makes sense if it can be done in an hour. After this time, the parasite is no longer of laboratory diagnostic value.
For the sake of comforting parents, it is worth noting that most people, even when bitten by infectious individuals, do not develop infections. From this point of view, the study of the mite for the carriage of bacteria and viruses is the most often useless exercise for the child and his parents.
Careful observation of the child during the month is required in any case. The body of the parasite, if it is decided not to take it to the laboratory, should be destroyed.
If it is decided to send the tick to a study, then it is necessary to put a piece of wet cotton in the jar. Mite at the time of delivery must be alive, corpses are not examined.
Treatment
After the bite, the child is usually given prophylactic doses of two. antibiotics - "Doxycillin" and "Ceftriaxone».
The first drug is taken during the first five days, the second - three days. Even if borrelia infection has occurred, these drugs help prevent the disease in 90% of cases.
To protect your baby from encephalitis, in the first 72 hours, you can enter a special serum - tick-borne immunoglobulin. It is available in every hospital, in any emergency room.
Reception is often recommended for children. "Anaferona"However, recently, this prescription raises many questions, because the drug is homeopathic and its effectiveness has not been clinically proven. Much more efficient and smarter to take «Rimantadine" or "Tamiflu».
Medicine also gradually began to refuse the introduction of serum, since it too often causes allergies in children.
External agents, such as "Fenistil". Other medications do not need to be taken. If, after 11 days, blood tests using the PCR method show the presence of tick-borne disease, the doctor will prescribe the appropriate treatment in-patient or out-patient.
Prevention
If you are going for a walk in the forest, make sure that the child’s clothes are not too dark - it will be difficult to see a tick on it if it appears. Walking in the season should be carried out in closed clothes, which covers the arms, legs, neck. The head of the child must be protected by a hat.
There are many repellents from ticks, there are also separate children's preparations. In campaigns for mushrooms or berries, as well as sending a child to rest in a country camp, be sure to stock up on such means.
In the shade ticks are always more than in sunny open spaces. You should not make halts and picnics in the shade of trees, it is dangerous.
Next to the paths, ticks are always much larger. They for 10 meters feel the approach of the victim, and for a long time they “understood” that hunting on the paths is very productive.Therefore, you should not sit on the grass, lying in it near the trodden paths.
If you are traveling or traveling with your child to the regions and countries with unfavorable conditions for tick-borne encephalitis, 2 months need to be vaccinated, after 30 days the vaccination is repeated. If the departure is urgent, and the two-month wait is not included in the plans, you can contact the clinic and enter the dose of immunoglobulin, it should be enough for about a month.
You should always have the preparations mentioned above: tweezers, thread, antiseptics. If the bite is found far from civilization, you now know what to do.
Prevention of tick-borne infections and officials are concerned at the state level.
In regions where tick activity is higher, at the beginning of the season, acaricidal treatments of places of mass visits — parks, forest parks, alleys — are carried out. Such a measure reduces the incidence of infectious diseases transmitted by arthropods, several times.
How to help a child after a tick bite, says Dr. Komarovsky in the next video.