Defect of the interatrial septum of the heart in children (DMPP) - heart aneurysm
If the doctors diagnosed a defect in the septum separating the atrium, this causes the parents to worry about the life of the baby. But instead of panic, it will be more constructive to learn more about the defect found in the infant in order to get information on how to help the child and how this heart pathology threatens him.
What is atrial septal defect?
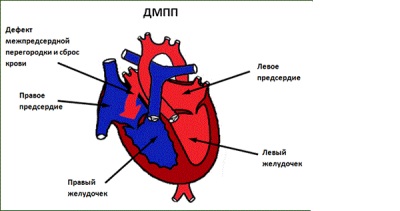
So called one of the congenital heart defects, which is a hole in the septum through which blood is discharged from the left half of the heart to the right. Its size can be different - and tiny, and very large. In severe cases, the septum may be completely absent - a 3-chamber heart is detected in the child.
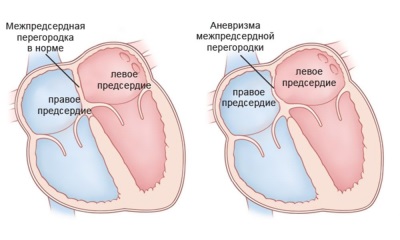
Also, some children may have a cardiac aneurysm. It should not be confused with such a problem as an aneurysm of cardiac vessels, since such an aneurysm in newborns is a protrusion of the dividing atrium of the septum with its strong thinning.
This defect in most cases does not constitute a particular hazard and, with its small size, is considered a minor anomaly.
The reasons
The appearance of DMPP is due to heredity, but the manifestations of the defect also depend on the impact on the fetus of negative external factors, including:
- Chemical or physical environmental impacts.
- Viral diseases during pregnancy, especially rubella.
- Use of the future mother of narcotic or alcohol-containing substances.
- Radiation exposure.
- Work pregnant in hazardous conditions.
- Reception during gestation of dangerous drugs for the fetus.
- The presence of diabetes in mom.
- The future mother is over 35 years old.
- Toxicosis during gestation.
Under the influence of genetic and other factors, the development of the heart is disturbed at its earliest stages (in 1 trimester), which leads to the appearance of a defect in the septum. This defect is often combined with other pathologies in the fetus, for example, a cleft lip or kidney defects.
Hemodynamics in DMPP
- In utero, the presence of a hole in the septum between the atria does not affect the function of the heart, since through it the blood is thrown into the systemic circulation. This is important for the life of the crumbs, because its lungs do not function and the blood that is meant for them goes to the organs that work more actively for the fetus.
- If the defect remains after delivery, blood during heart contractions begins to flow into the right side of the heart, which leads to an overload of the right chambers and their hypertrophy. Also, a child with DMPP over time, there is a compensatory ventricular hypertomy, and the walls of the arteries become denser and less elastic.
- With very large openings, changes in hemodynamics are observed already in the first week of life. Due to blood ingress into the right atrium and excessive filling of the pulmonary vessels, the pulmonary blood flow increases, which threatens the child with pulmonary hypertension. Pulmonary congestion and pneumonia are also a consequence of pulmonary congestion.
- Further, the child develops a transitional stage, during which the vessels in the lungs spasm, which is clinically manifested by an improvement in the condition.During this period, it is optimal to perform the operation to prevent vascular sclerosis.
Kinds
Defect in the septum separating the atria, is:
- Primary. It has a large size and location at the bottom.
- Secondary. Often small, located in the center or near the exit of the hollow veins.
- Combined.
- Small. Often asymptomatic.
- Average. Usually detected in adolescence or in an adult.
- Great. It is detected quite early and is characterized by a pronounced clinic.
- Single or multiple.
Depending on the location of the pathology is central, upper, anterior, lower, back. If, in addition to DMPP, no other pathologies of the heart have been identified, the defect is called isolated.
Symptoms
The presence of DMPP in a child can manifest itself:
- Heart rhythm disorders with the occurrence of tachycardia.
- The occurrence of shortness of breath.
- Weakness
- Cyanosis
- Lag in physical development.
- Heart pains.
With a small defect size in a child, any negative symptoms may be completely absent, and the DMPP itself acts as an accidental “find” during a planned ultrasound scan. If, however, with a small hole and clinical symptoms appear, it often happens during crying or physical activity.
With a large and medium-sized defect, symptoms may appear at rest. Kids because of shortness of breath hardly suck the breast, gain weight poorly, often suffer from bronchitis and pneumonia. Over time, they have deformed nails (they look like watch glasses) and fingers (in appearance they resemble drum sticks).
Possible complications
DMPP can be complicated by such pathologies:
- Severe pulmonary hypertension.
- Infectious endocarditis.
- Stroke
- Arrhythmias.
- Rheumatism.
- Bacterial pneumonia.
- Acute heart failure.
If such a defect is not treated, no more than half of the children born with a cerebral palsy live to 40-50 years of age. In the presence of a large aneurysm of the septum there is a high risk of its rupture, which can result in a lethal outcome for the child.
Diagnostics
On examination, children with such a defect will have an insufficient body mass, a protrusion on the chest ("heart hump"), cyanosis with large hole sizes. After listening to the baby's heart, the doctor will determine the presence of noise and the splitting of tones, as well as the weakening of breathing. To clarify the diagnosis of the baby will be sent to:
- ECG - symptoms of right heart hypertrophy and arrhythmia will be determined.
- X-ray - helps to identify changes in the heart and lungs.
- Ultrasound - will show the defect itself and clarify the hemodynamic problems that it caused.
- Cardiac catheterization - is assigned to measure pressure inside the heart and blood vessels.
Sometimes angio and phlebography are also prescribed for the child, and for diagnostic difficulties, an MRI is performed.
Is surgery necessary?
Surgical treatment is required not for all children with a defect in the septum that separates the atria. With a small size of the defect (up to 1 cm), its independent overgrowing is often observed by 4 years of age. Children with such DMPP are surveyed annually, observing their condition. The same tactic is chosen with a small aneurysm of the septum.
Treatment of children diagnosed with medium or large DMPP, as well as large heart aneurysm, is surgical. It provides for either endovascular or open surgery. In the first case, the defect is closed to the children with a special occluder, which is delivered directly to the heart of the child through large vessels.
An open operation requires general anesthesia, hypothermia, and connecting the baby to an “artificial heart”. If the defect is medium, it is sutured, and for large sizes, the hole is closed with a synthetic or pericardial flap.To improve the performance of the heart, cardiac glycosides, anticoagulants, diuretics, and other symptomatic agents are also prescribed.
The following video will provide you with useful tips for parents who have experienced this disease.
Prevention
To prevent the occurrence of DMPP in a child, it is important to carefully plan the pregnancy, pay attention to prenatal diagnosis and try to exclude the influence of negative external factors on the pregnancy. Future mother should:
- Fully balanced to eat.
- Enough to rest.
- Regularly go to the consultation and take all tests.
- Avoid toxic and radioactive effects.
- Do not use medication without a doctor's prescription.
- Protect yourself against rubella in a timely manner.
- Avoid contact with people with ARVI.