Streptoderma in children: from symptoms to treatment
Various skin diseases are not uncommon in childhood and adolescence. The immunity of the child is not as strong as that of an adult, and therefore often cannot give a decent immune response to the invasion of pathogenic microflora. So begins streptoderma - a disease widespread in childhood.
About the disease
Streptoderma refers to infectious diseases of the skin. It causes her streptococcal microflora. Streptococci live everywhere and are considered parasites. Most of them are in the digestive tract, in the mouth, in the nose and large intestine. Streptococcus sizes are small - about 1 micron in diameter. Breed very quickly. In the process of reproduction, bacteria produce toxins, and it is this fact that causes the disease - purulent rounded areas appear on the skin. Outbreaks of streptoderma may be small - just a few millimeters and large - up to 20-30 centimeters in diameter.
Since there are many types of streptococci, then under streptoderma should be understood several types of disease:
- contagious impetigo;
- bullous impetigo;
- angular stomatitis;
- simple lichen;
- tournamentol;
- streptococcal diaper rash.
In the world there is no accurate data on how common streptoderma, because patients do not always refer her to doctors. Many prefer to treat mild forms on their own, and therefore data on the diseased is not recorded anywhere.
It is known that streptococci more "love" women and children. According to WHO estimates, the prevalence of streptoderma in children and adolescents with dermatological problems reaches 60%.
How does the infection occur?
When asked whether streptoderma is contagious or not, there is only one answer - this disease is very contagious. The path of its distribution is called household contact.
A child can become infected with infection from other children and adults, playing with some toys, being in tactile contact, using common things, dishes, towels, and objects.
That is why most often the disease affects the whole children's team at once - in a kindergarten or school, in a group in a sanatorium or a children's camp. Similarly, adults are infected.
It should be understood that streptococcus in order to develop, we need an optimal habitat - a temperature of about 37 degrees with a plus sign, a special humidity. This environment is the human body. To get into a suitable breeding environment, the microbe must overcome the outer layer of the skin. It facilitates the task of any wound, scratch, abrasion on the skin of the child. The infection spreads very quickly.
Most often, the peak incidence occurs in the warm season - spring and summer. It is during these seasons that sweating increases, which in itself increases the likelihood of microtraumas of the epidermis.
The incubation period is difficult to determine a specific time frame, all very individual. From the moment the streptococcus hits the skin, if there are lesions on the skin, it takes from 7 to 10 days to develop the clinical symptoms of the disease (when characteristic features appear on the skin).
The child remains contagious as long as there are pockets of streptococcal infection on his skin.
Most often, one of the group of streptococcal diseases develops when a baby or teenager has some associated skin problems:
- pediculosis;
- dermatitis and dermatosis;
- scabies;
- allergy;
- teenage acne;
- reduced immunity;
- the presence of anemia;
- chronic illnesses;
- parasitic infections;
- violation of hygiene rules.
The disease occurs in toddlers and older children with almost the same frequency, but in kids it is harder, lasts longer. These are the age features of immunity. Causes of occurrence is not always possible.
In addition to the contact path of transmission, there is an airborne droplet, but in this way streptococcus is transmitted quite rarely.
Symptoms and signs
To determine the time of infection is usually very difficult, because during the incubation period there are no signs of the disease. Only in 7-10 days the initial stage of the disease is manifested - streptococcal formations. Each looks like a rounded pinkish color. It is not necessary that this element has the correct round or oval shape, often the spots do not have smooth edges.
After a few days, they begin to degenerate into purulent vesicles. It is the presence of pus that makes it possible to distinguish streptoderma from herpes or allergic dermatitis.. Depending on how deeply the microbes have penetrated, several clinical manifestations are distinguished: if the streptoderma is superficial (for example, with impetigo), the vesicles burst quickly and do not leave any marks, scars or scars after healing, and in the deep forms of the disease not only the epidermis is affected, but also the germ layer of the skin, which may result in the formation of ugly skin defects in the future.
In adults, the disease is almost not associated with any serious complaints of changes in health. But in children, streptoderma is more pronounced: there may be mild itching in the area of the affected areas, as well as dry skin at the site of the lesion. If the lesions are extensive, the child may rise to 37.0-37.7 degrees, there may be an increase in lymph nodes.
Streptoderma on the legs is often localized, but such an arrangement of eruptions and any other may well spread to the whole body in a short time. Individual elements can merge, forming even more extensive areas of damage. If only skin folds are initially affected, for example, on the pope, in the elbow folds on the arms, then there is every chance that a bacterial lesion will not go beyond the folds.
Even if the lesion is extensive, you should know that nails and hair are never susceptible to streptoderma.
If the affected skin area is regularly exposed to injury, rubbing, then the disease can become chronic. For chronic streptoderma necessarily prerequisites. Most often this form of the disease develops in diabetes mellitus, in kidney diseases, in any chronic diseases in a child, in genetic diseases. In this case, the disease will appear and recede in waves. In between the attacks, the skin of the affected area becomes rough, flaky, it is dry and may differ slightly from healthy color.
At first, for the first infection, streptoderma is always localized, and the parents' task is to do everything possible to prevent the infection from spreading to the healthy epidermis.
Water is dangerous. It is the contact with her that will allow the spots to crawl through the body. This is especially noticeable in the case when the first elements of streptococcal eruptions appear on the face (cheek, chin, lips, on the nose).
When washing in a few hours, new foci of infection form on the head (on the nose, on the eyelid, etc.).e.), as well as on the hands, with a slight swelling of the epidermis between the affected old elements and the new ones.
How to recognize the type of disease?
According to the characteristic symptoms, it is easy to determine not only the fact of a streptococcal infection, but also its appearance.
These are signs of the most common varieties of this bacterial disease:
Strep impetigo
The most common form of the disease that overwhelmingly, develops in the nose, on the face, on the hands and feet, on the exposed parts of the body. This is a surface streptoderma, which almost never has negative consequences from the point of view of aesthetics of the appearance of the skin.
At the initial stage, the disease is a small vial with muddy contents, the skin around it quickly turns red. Quite quickly, it opens, forming a dry or wet yellowish-brown crust. When the crust falls off, the skin beneath it has a brighter color, hyperpigmentation (bluish-pink) lasts for some time, and then passes without a trace.
The sooner treatment is started, the greater the chances that the disease will not spread. Treatment may take up to several weeks. The child remains contagious within 28 days from the moment of the appearance of the first vesicle-conflict (this is the name that the primary streptococcal element has).
Slot-like impetigo (zaeda)
This form of streptoderma confused with another is almost impossible - it is always located in the corner of the mouth, and only in isolated cases is the location in the corner of the eye or on the wings of the nose described. The conflicts in this case are small in size and lethargy - the bubble quickly breaks and leaves a slit-like wound-crack with a yellowish crust. She comes off, and the wound is exposed again. The disease often causes the child to complain of pain when eating, smiling, talking, drooling, itching in the affected place. Very often, zaeda is chronic.
It is extremely rare that such streptoderma is distributed elsewhere from the place of its initial appearance. It is well treatable, but may be complicated by the addition of a fungal infection, especially if there is caries, candidiasis of the oral cavity.
Bullosa impetigo
This form of infectious disease, which is characterized by severe, it usually affects the feet, hands and knees. At first, the child will form in these places large blisters filled with pus and serous fluid. They are very flabby, soft, easy to tear. After a rupture, not scabs with scaling, but real erosion are formed; in children, this whole process often takes place against the background of an increase in temperature and an increase in regional lymph nodes.
If the infection begins in a baby (in infants, newborns), signs of general intoxication are not excluded. The younger the child, the higher the likelihood of concomitant clinical signs of deterioration in the general condition.
Simple lichen
This form of children get sick more often than adults. Most often the disease starts in children's groups in the autumn and spring. Most It can often appear on the face around the mouth, on the chin, cheeks, on the hands, and least of all - on the leg.. Bubbles with liquid or pus are not formed at the same time, therefore, often depriving it is called dry streptoderma.
It appears as lesions whitish or pinkish in color with delineated boundaries. Inside the hearth is covered with grayish scales. Rashes itch and itch.
If a child sunbathes in the sun for a while, manifestations of simple depriving are reduced, but do not pass at all.
The tan itself is unevenly distributed, the skin takes on a variegated appearance - in the lesion focus, the skin remains lighter.
Turniol
The second name for this type of streptoderma is impetigo nail rollers. In children occurs infrequently. Primary blister flikten appears on the skin next to the nail plate. This is quite a painful condition. Inside the blister the serous fluid stops for purulent within 2-3 days. There is a disease and another name with which people are better acquainted - superficial felon.
Often, erosion or an ulcer develops next, and a loss of the nail plate can occur. In young children, with this form of streptococcal infection, fever develops, and regional lymph nodes may increase.
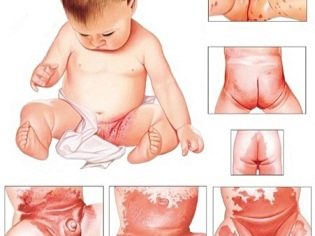
Streptococcal diaper rash
This form of the disease most often affects toddlers of infancy. Streptococcus affects the skin that already has signs of diaper rash or atopic dermatitis. Such the disease most often occurs in the ears and behind the ears, in the groin area, under the arms. The skin, which is most often subjected to friction, may also be infected with streptococcus (in women - under the mammary glands, on the inner thighs), in children - in the area of the buttocks.
Several small blisters with serous fluid appear, which quickly merge. They are painful, can itch and itch. After opening them, skin cracks and erosion are formed. In the absence of adequate treatment and with non-compliance with the rules of hygiene, chronic disease with occasional exacerbations is possible.
Diagnostics
The definition of streptoderma does not cause much work, even by visual signs. But the diagnosis in any case should be confirmed, but because parents who observe the skin of the child education, resembling an infectious skin disease, you should definitely refer to a pediatrician. It is best to pay a visit to the infectious diseases hospital, and not to the usual clinicAfter all, there are opportunities to quickly laboratory confirm or deny streptoderma.
As soon as the disease begins, it becomes possible to establish the presence of streptococcus by microscopic examination of bacteriological seeding of the scraping. This analysis is carried out first. With a scraping, streptococci are detected with an appropriate diagnosis. It is important to do this analysis before treatment, and therefore any self-treatment at home is highly undesirable.. If the mother tried to treat the disease in the child on her own, and then went to the doctor, scraping could be negative, whereas streptoderma will actually occur. But even in this case, an experienced doctor will distinguish this disease from other dermatological ailments by the combination of clinical manifestations.
The specialist will be able to distinguish it from the urticaria, pityriasis versicolor, pyoderma or dermatitis. At home, this is not always the case. Also in a hospital or clinic it is possible to determine the complications of streptococcal infection - fungal lesions.
If a child has had two or more episodes of streptoderma detection in the last year, it is strongly recommended to examine him comprehensively - examine the condition of the gastrointestinal tract, make an ultrasound scan of the abdominal organs, take tests for worm eggs, conduct laboratory blood tests for sugar, and thyroid hormones , and also make general blood and urine tests.
Treatment
If the child is fine with immunity (no HIV, severe autoimmune diseases), and the foci of the disease are single and non-extensive, usually local remedies are prescribed. In addition to such means, which directly treat the affected areas, it is recommended to take vitamins, UV therapy.
While parents will treat the child according to the recommendations of the doctor, you can not bathe the child. If necessary, to conduct hygienic procedures healthy skin can be wiped with a wet swab, trying in any case not to touch the affected areas. Can be used for such rubdowns not water, but a weak chamomile decoction.At the time of treatment, the child should not wear clothes made of synthetic fabrics, because it causes sweating, and sweating during this period increases the likelihood of the spread of foci of infection. To prevent this, we need not only clothes from natural fabrics, in which the skin will breathe well, but also the optimum air temperature in the room. In an apartment where it is hot, the child will sweat anyway.
A child from the first day of illness should have his own cup, plate, his own linen and towels. He should not play with other children, much less use the same toys and the same things with them.
Quarantine for streptoderma is 10 days. Therefore, after the discovery of the disease in a child, it is imperative to inform the kindergarten or school that the child attends. There must be a ten-day quarantine for all who had contact with the child.
For a child sparing diet recommended during treatment, devoid of any products with high allergenicity. Spicy and fatty foods should also be excluded from the diet. Food allergies during this period can lead to an increase in exudate and aggravation of the disease.
It is recommended to treat lesions several times a day.. If there are unopened bubbles, they are carefully opened with a sterile needle and treated with aniline dyes. For these purposes, the well-known brilliant green (brilliant green solution), melitenovo blue, "Fukortsin" is suitable for everyone. After this treatment, a clean, dry dressing with an ointment that has a disinfecting effect is applied to the site of inflammation.
If the child has formed a hard crust, in no case can not try to separate them manually, this can lead to the formation of severe eczema. Crusts are smeared with salicylic petrolatum and after about a day they are easily removed with the next treatment.
If streptoderma has a long and sluggish nature, antibiotic treatment is applied. The term usually does not exceed 6-7 days.
Drugs for therapy
Streptoderma in children is treated quite well and quickly, if everything is done correctly. A common parental mistake is to stop treatment as soon as signs of improvement appear. The course of treatment prescribed by the doctor must be completed completely without fail.
For local treatment, as already mentioned, the following drugs are used.
Brilliant green solution - a popular antiseptic, which is produced not only in liquid form, but also in a more convenient form - in the form of a pencil. It has not only an effect against bacteria, but also partially copes with some fungi, and therefore can be used for local treatment even with complicated streptoderma. Treat lesions twice daily.
"Fukortsin" - the second name - “liquid Kostellyani”, has a bright crimson color. The composition is effective against streptococci and some types of fungi. The skin treatment is carried out from 2 to 4 times per day. Before you apply the ointment, it is recommended to give raspberry liquid to completely dry on the skin.
Methylene blue, or just blue. This dye is used to treat affected skin up to 2 times per day. An alcoholic solution of aniline dye is available at any pharmacy.
You should not apply several dyes at once - the treatment for this will not become more effective. Choose one tool and don’t skip processing time.
If the lesions are large, they may additionally be recommended for pre-treatment before treatment with Miramistin and Chlorhexidine.
Ointments, which are often prescribed for streptoderma children.
Ichthyol - drug-antiseptic, which is especially effective for streptococcal eczema. Apply 2-3 times a day.
Tetracycline - A popular antibacterial drug for the treatment of skin diseases and eye diseases.For the treatment of streptoderma apply an ointment with a tetracycline concentration of 3%. It is necessary to use the lesion after treatment with aniline dyes 1-2 times a day.
Zinc. The main active ingredient is zinc oxide, which has a pronounced antiseptic and drying effect. On the basis of this substance, there are other drugs, for example, "Zindol". Especially effective for moist eczema.
Sulfuric ointment - A popular antiseptic that is active against most pathogens. Put on a previously prepared surface 1-2 times a day.
If the child has a tendency to allergies, antihistamines, such as Claritin, Suprastin, are also prescribed for the duration of the treatment. The exact dosage and number of doses per day prescribed by the doctor, depending on the age of the patient. If systemic antibiotics are recommended, then most often choose such means as "Amoxiclav" and "Flemoksin Solyutab." If a child has for some reason resistance to the penicillin group of antibiotics, Azithromycin or Summamed is recommended. In addition, prebiotics and probiotics can be prescribed in order to preserve the health of the intestines during antibiotic treatment.
Immunocompromised children (for example, a child shortly before streptoderma suffered severe influenza or ARVI or has chronic diseases with frequent relapses), therapy may be recommended by a doctor to maintain immunity. In addition to vitamins, it includes “Licopid” in tablets of various dosages (for kids, 1.0 mg each, for children from 15 years old - 10 mg each).
Opinion of Dr. Komarovsky
The famous pediatrician and TV presenter Yevgeny Komarovsky is sure that streptococcus is susceptible to any and all - the disease can occur in infants and adolescents, but it is more likely that it will manifest in a child attending a kindergarten or school involved in contact sports. Regardless of whether there are signs of a streptococcal infection on your finger or in any other place, antibiotics will help to quickly cure the ailment. Evgeny Olegovich strongly advises against giving up antibacterial therapy.
Unfortunately, many mothers mistakenly believe that it is possible to cope with streptococcus decoction of chamomile and calendula, as well as other "grandmother's" means, but this is not so. Streptoderma while it only spreads and becomes chronic. Modern antibiotics are not at all so terrible, and the harm from them is in many ways exaggerated, says Yevgeny Komarovsky, and this is also the most effective and quick treatment.
Projections for streptoderma are favorable, the disease is cured completely, easily. That is why it is absolutely useless to experiment with folk remedies if there are effective and quick ways of deliverance.
Prevention
Streptococci are the natural inhabitants of our skin. They have all - both in patients and in healthy people. They do no harm to a person as long as the immunity is strong enough. But if it weakens or damage occurs on the skin, the person automatically falls into the risk group for streptoderma. Knowing this, it is worthwhile to take care of the prevention of infection in advance. This will help you simple tips.
- Teach your child hygiene from an early age. More closely monitor the hygiene of the baby. As soon as the child came home, you should immediately wash your hands, approach the infant with clean, washed hands. If a child is in a crowded place for a long time, for example, traveling with his mother on a train or by plane, then you should not only wash your hands, but also treat them with an antiseptic, for example, "Miramistin".
- It is best to treat any scratches, abrasions and sores in a child immediately with an antiseptic.For example, hydrogen peroxide, without waiting for an infection or not.In case of injury, you can apply the cream "Baneotsin" or another therapeutic and prophylactic drug.
- Chronic diseases increase the likelihood of susceptibility to bacteria, and therefore leave them on their own course should not be in any case., the child must receive timely and proper medical care.
- Strengthen children's immunity. Children who grow up in “greenhouse” conditions suffer most often from various illnesses, including skin infections. Adequate physical activity, sports, walking in the fresh air, hardening and healthy food without overfeeding are the best way to support the child’s immunity.
- Children from an early age should be taught not to take other people's objects., toys and not to give to the use of unfamiliar people own things.
Especially it is necessary to be attentive in the event that the child already had been ill with streptoderma. This specific pathogen does not produce immunity, there is no vaccine from it, and therefore repeated infection is very, very likely. Therefore, it is very important to be sensitive to the news from the kindergarten, school. If talking about quarantine, be especially vigilant, inspect the child daily. If your baby is sick, do not hesitate - be sure to inform the leadership of the preschool or educational institution.
Observe restrictive measures - do not carry a sick child in public transport, you can walk with him, but not on the playground where other children walk, but in the distance, in a park or a public garden, where the child will not contact peers, touch slides, carousels, benches.
Reviews
Quite a number of forums are devoted to discussing childhood streptoderma - parents share their experiences and advice. Many mothers believe that streptoderma should be treated as soon as possible, because long-term treatment with the formation of eczema and cracks increases the likelihood that ugly scars and scars will remain on the baby’s skin.
The most positive reviews are about Fukorcine, Levomekol ointments, tetracycline, erythromycin and other antibiotic ointments.