Fetal heartbeats by week: features and norms in the table
Fetal heartbeat is an important characteristic that allows doctors and mother to understand how well the baby feels in the womb. They begin to measure it before other parameters of life and continue throughout pregnancy and childbirth. In this regard, moms have a lot of questions about heart rate.
How is the heart formed?
The heart of the baby begins to form one of the first. The woman still does not realize that she is pregnant, and the crumbs are already undergoing intensive processes of organogenesis of the heart and great vessels. This process begins in the second week of pregnancy. (from the date of conception).
In the embryo in the first week of its existence, two heart germs are formed - endocardial tubes. They gradually merge into one, but two-layer. The most rapid growth of the tube occurs at 3 weeks of pregnancy (first week since the start of menstruation). Despite its miniature size, the embryo's heart tube has a rather complicated structure: it has five sections, of which the atrium, ventricle, venous sinus will be formed, there is an arterial bulb and a trunk.
The child’s heart gets a characteristic appearance at 5 weeks from the day of conception., that is, at 7 obstetric week. At this point, the heart is already divided into right and left halves, separated by two partitions.
It is noteworthy that the formation of the heart does not occur where this organ is usually located, but in the cervical region. As the organ develops, it gradually descends to where the chest will later be. On the way there, the heart turns over, and those departments that were formed from above are at the bottom.
This process is very complex, and therefore any violations in it can cause a gross pathology, for example, the heart will remain in the cervical region or not turn over, and then its tip will be turned down.
At week 4 of embryonic development, the ventricular septum is formed, the organ is divided into 2 parts. At the 6th week of development of the baby, an oval window is formed in the partition and the heart becomes a three-chamber. At week 7 begins and by the end of week 8 the process of the formation of another septum is completed and the heart becomes a four-chamber, like in each of us.
The fetus begins to beat the heart at the end of the 5th week of pregnancy, this can be fixed by the results of ultrasound. There are no other ways to hear a tiny heart knocking in the early stages.
The period from 2 to 8 weeks of the embryonic period (from 4 to 10 weeks of gestation) is critical.
With any teratogenic factor, the formation of the heart and blood vessels may be impaired, which is fraught with the development of defects, sometimes incompatible with life. Such an influence can be harmful habits of women, adverse environmental conditions, harmful factors of production, etc.
When and why measure?
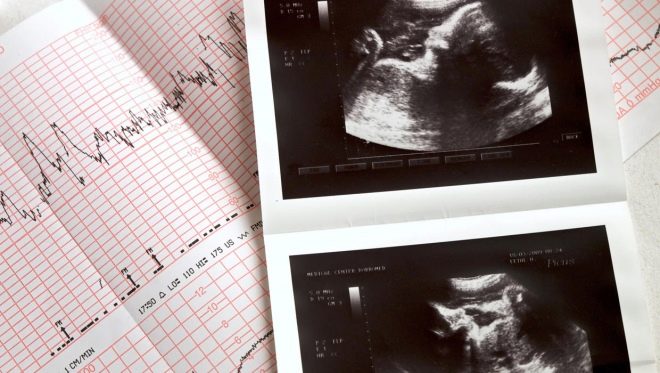
From the end of the 5th week to the very moment of birth, the fetal heart rate is measured at each ultrasound examination. This is not a tribute to tradition, but an important characteristic of the state of the baby at the time of the examination.The frequency with which the heart cuts out knocks in the ultrasound protocol is indicated by the abbreviation HR - heart rate.
Additional methods of listening to children's heart appear at different periods of pregnancy. From about 18 obstetric weeks, echocardiography can be performed. Doppler and color ultrasound gives an idea not only of how well the heart is shaped and how it knocks, but also of how blood circulates in the great vessels.
From the middle of the second trimester, the method of auscultation is used - listening with the help of an obstetric tube with a wide distal end (stethoscope). This is in the office of each obstetrician-gynecologist and with the procedure of listening begins, usually every planned reception of a pregnant woman. This method does not allow to calculate the heart rate in a numerical value, but gives the doctor an idea of how rhythmically and clearly knocks the heart of the child, as well as assume its presentation - when a heart beat is found below the navel, women talk about the head presentation, with a beating in the navel, to the right or to the left of it, suppose a transverse disposition of the crumbs, and if the heart is beating is heard above the navel, it is more likely that the baby is in pelvic presentation.
But the method is not too accurate, especially in case of polyhydramnios, when heart rhythms are poorly tapped, during low water, during pregnancy are twins or triplets, and also if the mother has obesity or when the placenta is located on the front wall.
From the 30th week of pregnancy another method becomes available - CTG (cardiotocography). It is done both according to indications, and to control all expectant mothers. The method is based on the registration of two indicators with sensors - the heartbeat and fetal movements are recorded, and the relationship between the movements and heart palpitations is monitored (this is typical of babies).
In the process of childbirth, it is also often necessary to register the heart rate and contractions by attaching the sensorium of the CTG apparatus to the pregnant woman's mother. This monitors the condition of the fetus in the process of delivery.
At home, you can hear how a baby’s heart beats, a woman can in several ways, but all of them are intended solely to satisfy curiosity — her own and the future father. A woman needs special medical knowledge to understand what this or that change in the rhythm of a child’s heart beats means. This is not about situations where home control of the heart rate is recommended by a doctor - in this case, use special portable fetal monitors, which temporarily give the expectant mother so that she can follow the doctor's recommendation.
An obstetric stethoscope can also be used for home listening after 24 weeks of pregnancy., but such a method is not available to the woman herself, because someone else will listen, for example, her husband. Fetal dopplers, small instruments with an ultrasonic sensor, are on sale today. You can use it at home from 13-14 weeks of pregnancy.
The main difficulty is to find the listening point, as practice shows, it does not work right away. You can use the usual phonendoscope - after 32 weeks of pregnancy, or try to listen to the baby's heart through the abdominal wall, but for this, the baby should be conveniently located - facing the abdominal wall.
Heart rate is an indicator about which doctors do not have a unanimous opinion. It is often believed that it does not have a high diagnostic accuracy, since the reasons for which the heartbeat can slow down or accelerate can be many, and even the usual excitement of the mother or her poor state of health will necessarily affect the heart rate. Why, then, measure the heart rate?
First of all, for the diagnosis of pregnancy itself - at week 5. A small fertilized egg may be imperceptible in the uterus, but its beating and the characteristic sound will not allow the doctor to look at the crumbs.Secondly, the baby's heart muscle responds to any changes in its state, which may be important as part of a comprehensive assessment of the fetus. As an independent measure that allows you to make a diagnosis, the measurement of heart rate does not act. But advantageously complements the information that can be collected during the ultrasound, laboratory tests.
But in the process of the birth of the baby in the hospital, the measurement of heart rate is a direct indication of his condition. Acute hypoxia in the process of childbirth is very dangerous for the child, and the predictions will depend on how quickly the doctors learn about it and decide on the future management of the birth.
Norms
Before talking about the heart rate standards, it is important to understand that in the process of forming the cardiovascular system, the baby's heart knocks unevenly. After 8 weeks the rhythm usually becomes more confident, clear.
Much in this parameter individually. If a woman suffers from toxemia or has a cold or colds, the baby always has a fast heartbeat, and an examination during this period will give inflated figures. If the mother lay on her back for a long time, as a result of which the vena cava was squeezed by the pregnant uterus, the heart rate may be reduced, but after changing the position of the body, it will return to normal again after a while.
The child in the womb sleeps and is awake, and in these two states he has a different heart rate.. In the later stages of pregnancy, the baby is quite emotional, he hears a lot, feels, may experience fright, and the heart muscle first responds to this and gives inflated readings of the heart rate.
The rates for early and late dates are different, as can be seen from these tables.
Table of normative values of heart rate - early terms
Term week | Heart rate range (beats per minute) |
5 | 80 – 103 |
6 | 101 -127 |
7 | 125 – 149 |
8 | 149 – 173 |
9 | 150 – 195 |
10 | 160-180 |
11 | 150 -180 |
12 | 148 – 177 |
13 | 145 – 173 |
14 | 146 – 169 |
Table of normative values of heart rate - the second half of pregnancy
Term week | Heart rate range (beats per minute) |
15 – 32 | 130 – 160 |
32 – 38 | 140 – 160 |
38 – 42 | 120 – 160 |
Can these norms be considered as rigid? No, because a huge number of factors can affect the heart muscle of the crumbs. Slight deviation of the heart rate in one direction or another is completely allowed.
If a doctor has certain concerns about the health and condition of the baby based on the results of the heart rate, he will definitely prescribe additional tests.
Deviations and causes
And yet, the inconsistency of the heartbeat of a child's heart with average norms cannot but frighten women. Hearing from the doctor that the heart rate does not correspond to the norm, the expectant mother begins to worry, what aggravates the situation even more - during stress in the female body there is an increased production of adrenaline and cortisone (stress hormones), which does not go unnoticed by the heart muscle of the crumbs. Therefore, let's calmly consider the possible causes of deviations from the norm.
Decreased heart rate
Your baby was diagnosed with bradycardia. Heart beats slower than necessary for the duration of pregnancy. Most often this happens in the final, third trimester, when the baby becomes closelywhen the placenta begins to age and worse to cope with its gas exchange and nutritional functions.
Fetal bradycardia is considered a condition in which the heart rate is reduced to 110 beats per minute and below. Please note that during CTG, the heart rate may drop to such values, but then it returns to the original numbers. Bradycardia - persistent reduction in heart rate, which is observed throughout the entire survey.
Bradycardia itself does not indicate any particular disease, but doctors treat it very carefully, as it always says that the child’s condition is significantly disturbed. Slow fetal heart rate can be heard if a woman leads an unhealthy lifestyle - smokes, takes alcohol and narcotic substances during gestation. Often the baby's heartbeat slows down due to the mother’s anemia. (It is for this reason that the deviation of the heart rate in the direction of decrease is observed more often in the third trimester)
If a woman has little or no water, then the fetus can also be disturbed. Violation of the amount of amniotic fluid is diagnosed quite easily, and the entire pregnancy for such women is most closely monitored. The reason may be a woman taking drugs with a hypnotic effect, the abuse of sedatives. Sometimes persistent bradycardia indicates congenital malformations.
The slowed frequency of the beating of a child's heart is always an alarming sign, since it indicates that the baby is in a state of decompensation, that is, the disorder is at least chronic, and the body of the baby no longer has the resources and ability to compensate for what it does not receive. Bradycardia may suggest severe intrauterine chronic hypoxia (oxygen starvation) placental insufficiency, placental infarction, severe Rh-conflict in a Rh-negative woman with a Rh-positive child, mechanical asphyxiation of the umbilical cord (entwined around the neck).
The reaction of doctors to bradycardia should be immediate. It is necessary to establish as soon as possible the cause that led to the condition and eliminate it.. If it is not possible to establish or eliminate it, an early caesarean section is carried out to save the child’s life and in its interests.
The only case in which bradycardia is not an indication for emergency hospitalization is the identification of a slower heart rate due to a temporary circulatory disorder. (squeezed vena cava, squeezed by the child inside the uterus umbilical cord). Usually, a woman is asked to walk and walk for half an hour, to return and undergo an examination again. Physiologically related bradycardia with repeated examination is not confirmed.
If again the results of the heart rate are low, the woman is hospitalized, since her condition and the condition of the baby can at any time require medical intervention.
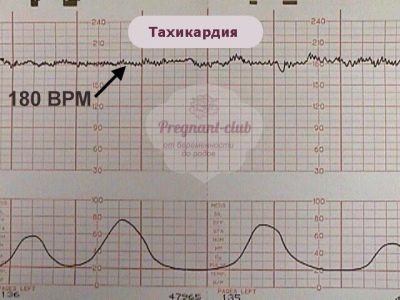
Increased heart rate
Inflated rates of fetal heart rate are less dangerous than lower ones. Already it was said that fear, stress may well be the cause of such results of the survey. But even if it's not about stress, often a beating heart is a sign that the baby is struggling, his condition is compensated. High values of heart rate are called tachycardia, they say about it, if the heart rate exceeds 175 beats per minute. Deviation should also be stable, persistent. The exception is the period from 8 to 11 weeks of pregnancy, when the high heart rate is a physiologically determined rate.
The reason for the increase in frequency may be bad habits of the mother, as well as some of her diseases. For example, with hyperfunction of the thyroid gland, when the level of its hormones increases, a change in the heart rate of both the baby and his mother may well be observed. In case of severe toxicosis, if vomiting becomes habitual for a woman, the likelihood of dehydration increases, and in this case, the baby’s heart is heard with the definition of tachycardia. The cause of fetal tachycardia can be maternal heart disease, impaired functioning of her kidneys.
A child may have his own personal reasons for frequent heartbeat - structural violations of the placenta (its defects), the presence of intrauterine infection, hypoxia in the initial stages.
Oxygen starvation, if it began recently, is perfectly compensated by the children's organism, forcing its adrenal glands to work a little more actively. While the state is compensated, the heart rate is increased, as soon as after that bradycardia occurs, they say that the condition of the fetus has worsened - he stopped struggling and compensated for the lack of oxygen. In the absence of urgent assistance, he may die.
It should be noted that some chromosomal abnormalities also tend to be too frequent heartbeat. For example, a fetus with Down syndrome often suffers from concomitant tachycardia.But for the diagnosis of chromosomal abnormalities to listen to the heart a little, for this there is its own system of diagnostic measures.
Boy or girl
Speaking of fetal heartbeat, it is difficult not to dwell separately on the topic of determination sex future child's heart rate. Despite the fact that the court is the 21st century, many people still believe that the frequency of the heartbeat of a child can indicate the sex of the fetus. They believe because they want to believe, and it’s impossible to determine the sex of the baby in the early stages - an ultrasound scan of 15-16 weeks cannot reliably answer the question of what gender a woman is waiting for.
Experts say that there is no relationship between the sex of the baby and his heartbeat.. Sex crumbs formed at the time of the merger of the germ cells of the parents. If the last pair of chromosomes coincide in type XX - a girl will be born, if XY is a boy. Organogenesis of the heart occurs equally in the embryos of both sexes., the organ and its functions develop equally in weeks, otherwise doctors would have two diagnostic tables - one with heart rate for boys, the other - with heart rate for girls.
At the same time, women's forums are overflowing with messages and discussions of this issue, as if no one hears the opinion of specialists. The girl is credited with a more frequent heartbeat, boys are more rare. In girls, say experts on folk methods of determining sex, the heart beats confusedly, indistinctly, and in boys the rhythmically. In fact, the confused and fuzzy rhythm of the heartbeat of a child’s heart appears only in one case - if the child has congenital heart defects.. And it makes no difference whether the boy is inside the womb or the girl. Sick hearts really knock with differences from healthy ones.
If the child is healthy, then its gender doesn’t matter - the heart will be beating rhythmically and clearly both in girls and boys.
To find out the gender, if this is important, it is necessary to do an ultrasound scan for a period after 14 weeks or donate blood as part of a non-invasive prenatal DNA test.. Ultrasound gives the answer with an accuracy of 80%, DNA test - with an accuracy of 99%.
One more a common myth about heart rate says that during pregnancy after IVF with a cryoprotocol, babies' hearts beat more slowly. As can be seen from the above, this is not true. Cryopreservation of germ cells and embryos reduces their viability, but does not affect the development of the embryo if the implantation is successful.
Attentive mothers listen to the heart of their crumbs during an ultrasound scan or at home on their own with the sinking of their own hearts, tenderness and tranquility appear, the woman’s stress level at that time decreases and this is true.
The sound of a child's heart is an indisputable sign of a new life inside. To know about it is one thing, but to hear is quite another.
You will learn about how the heartbeat is recorded on the results of an ultrasound scan at week 7 of burden, in the next video.