Dacryocystitis in children
Tearing and festering eyes in a child is not a sight for faint-hearted parents. Even without special medical knowledge, moms and dads understand that in this situation something needs to be done. After reading this article, you will learn about one of the reasons - dacryocystitis in children, as well as how to help your baby.
What it is?
Dactriocystitis is an inflammation that occurs in a special organ whose function is to accumulate tears (the lacrimal sac). This organ is located between the nose and the inner corner of the eyelids. Tears are produced in all people - as a natural, by the nature of the prescribed antiseptic and protective mechanism for the organs of vision. The excess of this fluid normally flows through the nasolacrimal duct into the nasal cavity and out.
If the lumen of this nasolacrimal canal is disturbed, then the outflow is very difficult. Tears accumulate in the bag - in the corner of the eye, which is why the eyes look watery. Inflammation and decay occur due to the multiplication of pathogenic bacteria. Stagnant biologically active fluid for them is an excellent breeding ground.
Inflammatory changes in the lacrimal sac may be caused by eye injuries, infection of the eyes, and narrowing of the nasolacrimal canal is a consequence of eye disease or a congenital feature of the newborn. That is why dacryocystitis is often called the illness of newborns.
In ophthalmology, these two types of ailment decided not to combine, because dacryocystitis of newborns is a more physiological problem, which is solved as the child grows. And dacryocystitis in general (for example, in older children) is a pathology that must be dealt with in a completely different pattern.
Dacryocystitis, which does not occur in infants, can be acute and chronic. And in the acute form often there is phlegmon or abscess of the lacrimal sac.
The reasons
In newborns, the nasolacrimal canaliculi are very narrow, the lacrimation is disturbed due to the congenital underdevelopment of the lacrimal ducts, which have not been absorbed by the gelatin tube in time. Dacryocystitis of the newborn is considered the most favorable from the point of view of prognosis, since it often passes on its own, without serious therapeutic measures.
In older children, the risk of developing obstruction and partial obstruction of the nasolacrimal canal increases during the incidence of ARVI or influenza, as well as other respiratory illnesses that cause swelling of tissues in the nasopharynx.
Obstruction of the lacrimal ducts may appear as a result of chronic or prolonged rhinitis, with adenoiditis, with allergic rhinitis, as well as with a bacterial infection.
If a child has a curvature of the nasal septum, which occurred due to a fracture of the nasal bones, if he has polyps in the nose, the risk of developing dacryocystitis increases significantly.
The mechanism of development of the disease is about the same (regardless of the original cause): first, because of the swelling, the patency of the lacrimal canal is disrupted, then tears accumulate in it and in the lacrimal sac. The protective properties due to the lack of circulation are lost quite quickly.
Then everything depends on which pathogen microorganism settles in this development-friendly environment. It may be a viral agent, or a bacterial flora, or parasites, or even chlamydia.
In response to the stagnation of fluid, the lacrimal sac begins to stretch, grow in size, so an abscess or phlegmon is formed.
Symptoms and signs
In dacryocystitis, the symptoms are quite specific, and it is rather difficult to confuse them with signs of other eye diseases. Usually in children, the disease is one-sided - only one eye falls ill. Only in 3% of cases dacryocystitis is bilateral.
The chronic form of the disease is manifested by increased tearing, as well as some visual swelling of the lacrimal sac. If it is easy to press on this swelling, a cloudy or purulent fluid may start to stand out.
The consequences of this form of dacryocystitis can be rather unfortunate, since inflammatory processes can pass on to other membranes of the organs of vision, and diagnoses such as keratitis, blepharitis, and conjunctivitis can be made to the child. There may be a thorn.
In the acute form, dacryocystitis is more pronounced. The eyelid becomes red and swollen, the area of the enlarged and inflamed lacrimal sac (in the inner corner of the eye) becomes painful to the touch. The edema can be so extensive that it will cover both the upper and lower eyelids, and the child will not be able to open the eye.
In some cases, it is rather difficult to determine the true focus of inflammation, since it does not have clear boundaries, it can “spread” to the orbit of the eye, and on the cheek, and on a part of the nose. The child complains of poor health, the temperature may rise, chills begin, signs of fever and intoxication are likely.
This condition usually lasts for several days, after which the skin in the region of the lacrimal sac begins to change color, it turns yellow and becomes softer. This is how an abscess begins to form. In most cases, it opens up on its own, but here lies a new danger - pus can spread to the fiber and cause phlegmon.
In newborns, dacryocystitis is less pronounced. When it does not increase the temperature, usually does not form an abscess. Parents may notice that the baby "sour" eye.
This is especially noticeable in the morning, after a long night of sleep. The eyes of a baby are watery and turbid. With a slight pressure on the lacrimal sac, a small amount of muddy secretions can be released, sometimes - pus.
Blockage of the nasal channel and subsequent inflammation of the lacrimal sac is not a contagious disease. Although upon detection of the signs described above, parents must take the child to see an ophthalmologist.
Diagnostics
It can be quite difficult for parents to independently examine the child, since the baby can desperately resist attempts to put pressure on the inflamed lacrimal sac. However, not every mother will risk doing it on her own. Therefore, an examination by an ophthalmologist always begins with palpation of the lacrimal sac and determination of the nature of the discharge.
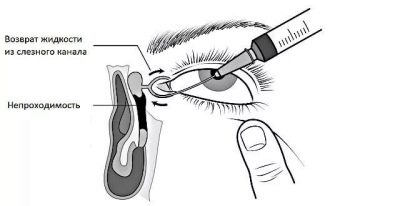
To confirm the diagnosis, use a special technique, which was called the "canalicular test West." The nasal passage on the part of the affected eye is tightly closed with a cotton swab, and a contrast agent is instilled into the eye (a collar solution).
With the passage of the tubule in a minute or two, traces of coloring matter appear on the cotton ball. In case of obstruction, the cotton wool remains clean. In case of obstructed circulation, which occurs when the lacrimal canalicus narrows, traces of the collargol on the tampon appear with great delay. That is why the test West is evaluated not only after 2-3 minutes, but after 15 minutes, if there were no traces of dye on the tampon for the first time.
To determine the extent of blockage or contraction, doctors can conduct diagnostic probing. During the procedure, the tear channel will be flushed. If the fluid will only flow out of the eye and not get into the nose, doctors will be able to determine at what level the obstacle occurred.
If dacryocystitis is confirmed, then the doctor will need to find out another important nuance - which microbe or virus began reproduction in the overflowing lacrimal sac.
To do this, smears of the contents, which is released during palpation, are sent to a bacteriological laboratory for analysis. This allows you to establish the exact name of the pathogen, to prescribe an adequate and effective treatment.
In difficult cases, other specialists are also invited to treat the ENT, the surgeon, the facial surgeon, the neurosurgeon and the neurologist.
In a newborn and an infant, diagnostic actions are usually carried out in a simplified manner - it is enough to be examined by an ophthalmologist and analyze the contents of the lacrimal sac on the baccephalon.
Treatment
In infants
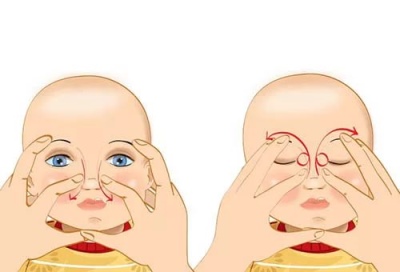
When it comes to newborns and infants, there is usually no need for inpatient treatment. Since the condition is due to physiological reasons, it is enough to make a karapuzu daily massage of the tear ducts. The massage technique is quite simple, and the procedure allows more than 90% of children with such a diagnosis to successfully recover in this way, without any other medical intervention and the use of strong medicines.
To properly massage, you do not need to go to special courses.
Mom should get rid of nail polish and do all the manipulations with clean hands, so as not to infect the child.
Massage begins with light tapping movements in the region of the lacrimal sacs (it is better to do a two-sided massage). Then the thumbs should be 10-15 times in the direction of the tear duct (with a slight touch). The direction is simple - from the corner of the eye to the nose. It is very important that the movements be exactly from top to bottom, and not vice versa.
The massage session ends with a vibrating motion in the region of the lacrimal sac.
The discharge of pus or turbid fluid from the corner of the eye, where the lacrimal punctures are located, should not be frightening. This fact rather suggests that the manipulations are done correctly.
It is recommended to repeat the exposure several times a day - for example, before feedings, but not more often 4-5 times. After each such session, you can drop a furatsilin solution (1: 5000) or “Miramistin"At a concentration of 0.01%.
Usually, this treatment is enough to get rid of dacryocystitis completely. When there is no relief, and the inflammation begins to progress, doctors prescribe a sounding - a manipulation that allows you to restore the patency of the lacrimal-nasal canal.
Sounding is carried out under local anesthesia (or by preliminarily introducing the child into a state of drug sleep). The essence of the intervention is reduced to the mechanical release of the nasal duct. For this, a special probe is initially introduced into the channel. Due to its conical shape, the probe not only eliminates the "blockage", but also expands the channel itself.
Then a long probe is introduced and the patency is checked along the entire length. It breaks adhesions, if any, pushes the cork out, makes the canal all the way clean and free. The procedure ends with the introduction of antiseptics, washing. After that, the doctor again conducts the color test Vest, described above, to check whether the patency is restored.
Other children
Acute dacryocystitis, which has arisen under the influence of various factors at an older age, is treated in a hospital - under the supervision of specialists. While an abscess is ripening, only physiotherapeutic methods are used - UHF and compresses with dry heat on the lacrimal sac.
When an abscess appears, it is opened, the tear sac is emptied, and treatment is prescribed, depending on the type of pathogen. If the inflammation is bacterial, prescribe antibiotics in the form of eye drops or an ointment with antibiotics. In viral infection produce treatment with antiseptic solutions.
Quite often, with bacterial damage (and it is the most frequent), systemic antibiotics are prescribed in pills or syrups. When the acute period is left behind, a decision is made about the feasibility of an operation to restore the patency of the lacrimal canal.
The most commonly used drugs for the treatment of pediatric dacryocystitis:
- «Tobrex"- eye drops with an antibiotic;
- "Vigamoks" - antibiotic eye drops;
- «Vitabact"- eye drops with an antibiotic;
- «Levomycetin"- antibacterial eye drops and eye ointment;
- «Albucid"- antibacterial drops in the eye;
- «Miramistin"- antiseptic;
- «Cypromed"- eye drops with an antibiotic;
- "Oriprim-P" - eye drops and ointment.
For all children prescribed multivitamins, and with viral lesions - means to stimulate the immune system.
Chronic dacryocystitis can be treated only in one way - surgically. The operation, which is aimed at restoring the patency of the tear duct, is called "dacryocystorhinostomy". Since the clogged tear duct is sometimes already useless, surgeons are practically laying a new “channel” between the nose and the tear bag, which bypasses.
The operation is shown when neither the massage method nor the sensing have brought the desired result.
Dacryocystorhinostomy is not performed for children with acute forms of the disease, as well as during an exacerbation - especially if it is accompanied by purulent discharges.
The operation itself is performed under local or general anesthesia. It is very "jewelry", thin, demanding from the surgeon maximum accuracy and accuracy. After it, no cosmetic defects should remain, the child’s vision should not suffer.
The rehabilitation period takes about a month. All this time, the child needs flushing of the lacrimal-nasal canal, as well as instillation of drops in the eyes before bedtime. The most commonly prescribed anti-inflammatory drops, anti-bacterial agents, as well as vasoconstrictor drops in the nose (the first time after surgery), to increase the lumen of the vessels.
For at least 30 days after surgery, the child must observe a mode of restful activity.
It is contraindicated to him:
- bend down often;
- spend a lot of time in the cold;
- visit dusty and smoky places;
- do sport;
- touch your eyes with your hands.
Not always dacryocystorhinostomy passes "like clockwork". Sometimes during the operation unforeseen complications occur, and sometimes they manifest themselves already during the rehabilitation period. This is usually a hemorrhage into the orbital cavity, and the most common postoperative complication is the fusion of the tubule created by the surgeon and the recurrence of the disease. However, such complications do not occur very often.
Prevention
Prevention of obstruction of tear ducts in newborns does not exist as such, since the problem is usually congenital. However, you can prevent the transition to the chronic form by referring to a doctor in a timely manner and starting appropriate treatment.
For older children, prevention should consist in the timely treatment of all diseases of the upper respiratory tract, so that there are no prerequisites for blocking the tear duct.
Timely and correctly treated rhinitis is the absence of swelling in the nose, there will be no threats.
It should be carefully and carefully treat the organs of vision, to prevent their injury. It is important to teach the child not to rub eyes with dirty hands, not to do it on the street.
To learn how to massage the lacrimal canal, see the next video.