Fibrinogen rates during pregnancy
Maternal blood during pregnancy nourishes and provides the baby with everything necessary. Therefore, blood health is of great importance for the baby, for the mother, and for the process of the upcoming birth.
Numerous tests that a pregnant woman gives give the doctor a fairly complete picture of her state of health. Hemoglobin and platelet count are important. Also checked the number of febrinogen. About what it is, and how much it should be in the blood of the future mother, we will tell in this material.
What it is
When a person is threatened with blood loss, his body triggers a protective mechanism of blood clotting. And the key link in it is a protein called fibrinogen. It is produced by the liver, after which fibrinogen is completely dissolved in the blood plasma.
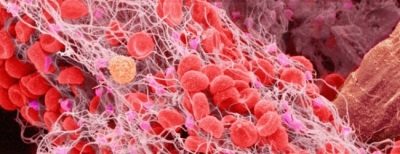
When injured, cut, surgery and other threats to the well-being of the body, fibrinogen begins to react with the enzyme thrombin. The result is a fibrin monomer.
It precipitates in the form of the finest threads that cannot be seen with the naked eye. These threads bind together blood cells, especially platelets. This forms a thrombus that completely covers the wound and prevents further blood leakage. Subsequently, the thrombus is absorbed under the influence of other substances, and the vessels are cleared of it.
During pregnancy it is important that blood clotting is normal. This will allow the child to get enough oxygen and nutrients, and mom - quietly convey the crumbs to the prescribed time and give birth to him without problems.
That is why the blood for clotting is checked several times during the carrying of the baby.
Fibrinogen assay
Fibrinogen is not the only indicator of the ability of blood to form blood clots, and therefore there is no separate analysis for it. The level of plasma protein is determined during a complex study of FPCM (soluble fibrin-monomer complex), which is also called a coagulogram.
Suitable for analysis venous blood only. Her fence is made several times during pregnancy, and then without fail before giving birth or holding a cesarean section. Doctors need to be sure that the woman does not have the risk of massive bleeding during childbirth.
The results of the analysis may be affected by some factors from the outside, and therefore before visiting the laboratory or treatment room. A woman should observe several important conditions:
- two days before donating blood, one cannot be nervous, worry, sort out relationships with relatives and strangers - hormones changing in stress will affect blood clotting;
- two days before the analysis you cannot eat fatty, spicy, over-salty or sweet foods;
- a few days should limit physical activity;
- blood thinners (eg aspirin) should not be taken a week before the test;
- blood is given on an empty stomach - the last meal of the future mother should occur no later than 8 hours before the blood is taken;
- if the expectant mother could not say goodbye to the bad habit of smoking, then one hour before the visit to the laboratory it is impossible to smoke.
The blood is placed in a test tube, treated with a special composition that prevents the formation of blood clots. In the laboratory, the plasma component is separated from it, and the amount of fibrinogen is determined in the plasma. For this purpose, special reagents are added to it, which trigger the thrombosis process in the sample. By the number of fibrin filaments formed, the laboratory technician judges the amount of fibrinogen.
Norms of values
Wise nature has provided everything for unhindered development in the womb of a new life. Therefore, at the very beginning of pregnancy and during the first trimester, fibrinogen in the blood decreases, so that the embryo can receive more beneficial substances, because blood flow increases.
At this time, the placenta is formed - and new vessels, including umbilical cord vessels, need to be treated with care and attention. For this maternal blood and becomes more fluid.
In the second trimester, when the vessels of the placenta and the umbilical cord become more durable and strong, and the basic laying of the organs of the child is completed, a new task appears for the mother's body - to prepare for the upcoming birth. That the risk of blood loss in the process of childbirth is inevitable, no need to say, this is obvious. Therefore, the blood begins to "thicken", the level of febrinogen increases, and consequently, the blood begins to clot faster.
The true danger in the process of childbirth - the discharge of the placenta. When a “baby seat” is born, it is always accompanied by bleeding. How abundant and controlled it will be depends on the time it takes to start a blood clot.
The number of febrinogen influences this indicator. Therefore, in the third trimester, the level of this plasma protein is normally always higher.
Table of standards for the concentration of fibrinogen during pregnancy by week:
Obstetric term (weeks) | Fibrinogen concentration - minimum | Fibrinogen concentration - maximum |
1-13 | 2.12 g / l | 4.33 g / l |
13-21 | 2.90 g / l | 5.30 g / l |
21-29 | 3.00 g / l | 5.70 g / l |
29-35 | 3.20 g / l | 5.70 g / l |
35-42 | 3.50 g / l | 6.50 g / l |
Causes of deviations
It should be noted that the level of fibrinogen during pregnancy is always slightly increased compared with the results of tests of non-pregnant women. However, the concentration of a substance in plasma may exceed the upper thresholds of the norm for women "in position", as well as deviate from them in a smaller direction. And the reasons for this may be enough.
If the level is elevated
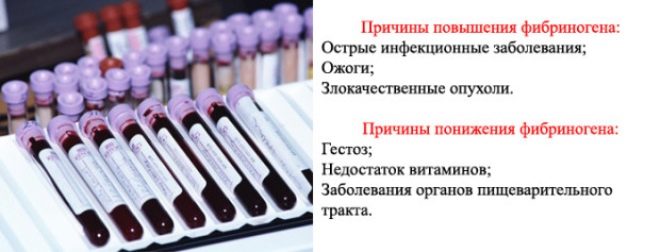
Excess febrinogen in the blood of a future mother can be caused by toxicosis or an infectious disease, because under these conditions the body loses fluid and becomes dehydrated.
To increase blood protein can bring transferred flu or ORVI, and also exacerbations of chronic diseases. Thicker blood also becomes due to severe stresses experienced by a woman, as well as if her activity is associated with serious physical exertion.
High concentrations of fibrinogen can talk about problems with the thyroid gland, diseases of the heart and blood vessels, pneumonia and rheumatism, as well as the development of thrombophlebitis in women.
The most alarming is the situation in which fibrinogen in the blood grows in response to malignant tumor processes.
Doctors with regret state that in recent years the number of women who have cancer problems are detected during the period of childbirth, is growing rapidly.
If the level is lowered
Low levels of plasma protein in the blood of the expectant mother may be due to gestosis, as well as due to a pathological deficiency of vitamin B 12 in her body.
Low fibrinogen and reduced fibrinolytic activity are characteristic of DIC (disseminated intravascular coagulation). This is a dangerous condition that requires expert medical attention. Reduced fibrinogen accompanies diseases such as hepatitis.
Plasma protein levels can be significantly reduced if a woman has recently suffered an injury, has suffered burns, has lost blood as a result of surgical interventions, and has also suffered poisoning with significant toxicity. As in the case of increased fibrinogen, toxicosis may be the cause of the decline.
Possible consequences
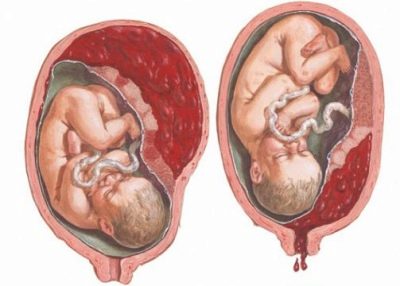
A slight excess of fibrinogen is easily treatable, and usually does not cause problems. A more prolonged and significant excess of the norm can cause spontaneous abortion, stop the development of the baby and his death.
Too thick blood increases the likelihood of uteroplacental thrombosis, which can lead to the death of the child in the womb. For the maternal organism, high fibrinogen poses a risk of thrombophlebitis and pulmonary artery thrombosis, which is fatal.
Due to excessively thick blood, the blood flow between mother and baby will be difficult, as a result, the baby will receive less vitamins, nutrients and oxygen, which can cause intrauterine growth retardation, as well as oxygen deprivation - hypoxia.
Reduced fibrinogen is detected in pregnant women much less frequently than elevated. This is a very disturbing sign, because A woman with "liquid" blood is threatened with bleeding and total blood loss. This can happen before birth, during childbirth, and in the postpartum period.
A hematologist will assist the gynecologist in the management of such a pregnancy, since such women need careful observation and a special approach.
Treatment
For the appointment of competent therapy of a coagulogram is not enough. Doctors need to establish the exact causes that led to deviations of laboratory analysis from the norm. For this, additional research is assigned - Ultrasound, ultrasound, CTG (if the problem is found in the third trimester of pregnancy), as well as other laboratory blood tests. You may have to visit a hematologist or transfusiologist to select medications for therapy.
What to do with a higher value?
If the increase in plasma protein is insignificant, it is enough to change the way of life and approach to nutrition, so that the blood clotting indicators normalize.
A woman is forbidden stress and heavy exercise. She should sleep for a sufficient amount of time (at least 9 hours) and observe the correct drinking regimen. At the same time, it is important to work out a tactic together with the doctor - how much water can be drunk per day so that there is no edema and dehydration.
The diet includes fresh tomatoes, sea buckthorn, cranberries, zucchini and cabbage. These products are good "thin the blood." Freshly squeezed red juices are useful, including vegetable, for example, beetroot.
Birch sap is very good (extracted from birch, not from a store). A woman can additionally be assigned vitamin complexes and separately - group B vitamins, folic acid, a small amount of aspirin daily.
Usually, such treatment is quite enough for blood clotting rates to return to normal within a couple of weeks.
If this does not happen, a hematologist who prescribes anticoagulants and individually determines the mode of their dosing is connected to the jurisdiction.
What to do at low rates?
As in the case of an increased level of fibrinogen protein, a woman is recommended to change lifestyle. Her diet includes foods that have the ability to thicken blood. These are bananas, baked potatoes, buckwheat porridge, chicken and quail eggs, pork liver, oats, walnuts and wheat.
Usually, “liquid” blood becomes on the background of late toxicosis, so a woman should not refuse from the hospitalization offered in this case to the hospital, where symptoms and intoxication will be removed with the help of medicines.
All drugs for the treatment of bleeding disorders are undesirable during pregnancy, but if there is no other way out, a woman can prescribe drugs - coagulants (hemostatics) calcium preparationsbecause this important mineral is involved in the blood coagulation process.
In order to minimize the risks for the child from receiving such funds by the mother, hemostatic therapy is tried to be prescribed as late as possible, closer to childbirth. It is carried out exclusively in the hospital under the supervision of a doctor.
It is not accepted to treat hemostasis problems with folk remedies: if the deviations are significant, medications are needed, not decoctions of herbs, especially since The use of most recipes recommended by non-traditional healers is also contraindicated in pregnant women.
For example, a decoction of nettle, which has a hemostatic effect, can cause "interruptions" in the uteroplacental blood flow, and the decoction of hypericum is generally contraindicated for women in an "interesting position."
Projections are usually favorable, especially since the current level of medicine allows the woman to provide all necessary assistance during childbirth and the postpartum period, even if the level of fibrinogen during the period of carrying the baby could not be normalized.
For more information about thrombophilia during pregnancy, see the following video.