8 week of pregnancy: what happens to the fetus and the expectant mother?
The early weeks of pregnancy are a very important period: at this time, many significant changes occur in the baby and female organisms.
How is the term determined?
In obstetric practice, a special system for calculating the age of the baby is used: doctors determine the fetal age of the baby in obstetric months and weeks. 8 obstetric week of pregnancy is equivalent to 6 weeks from the moment of conception of the baby.
Reviews of many women indicate that it is quite difficult for them to use the medical counting system to determine the age of the baby. Future moms, as a rule, use the calendar method of counting, counting the date directly from the date of fertilization.
To determine the obstetric period, doctors use the date of the first day of the last menstrual cycle. To do this, they will definitely check with the woman when she has a monthly delay. This method of counting is considered to be more accurate in medical practice and has been successfully used for a long time by obstetricians in different countries of the world.
So, the entire period of carrying a baby when using this method will be 280 days or forty weeks. The calendar system for calculating the age of the fetus from the moment of conception will differ somewhat from that used by obstetrician-gynecologists.
In order not to get confused, doctors recommend expectant mothers to also focus on the period defined in obstetric months and weeks.
Features a woman
In the first trimester of pregnancy, a wide variety of events begins to occur in the female body, which is largely due to the changing hormones. This leads to the fact that the expectant mother in this period of pregnancy begin to appear specific symptoms. Many women note that they feel changes in their bodies and sensations that they have not previously experienced.
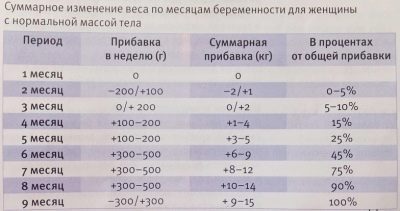
Actively developing baby in the womb promotes weight gain of the pregnant woman. In order to determine this indicator, doctors use the so-called weight gain. To do this, they carry out weighing during consultations.
Such a simple and effective method of examination allows the doctor to obtain indirect indications of how the child grows. For each period of pregnancy there are certain rates of weight gain.
During all months of childbearing the doctor enters this figure in the medical record of the future mother, which allows you to track the dynamics of the course of pregnancy, as well as to timely correct the resulting violations.
Almost daily in the female body changes in the concentration of hormonal substances.This feature is simply necessary to ensure that the intrauterine development of the child proceeds as it should.
The increase in the blood of female genital hormones contributes to the fact that the expectant mother manifests specific changes in the mammary glands. As a rule, by this period the halos become larger, the nipples become darker.
By this time the baby is carrying the breast most often increases by a few centimeters. Painful sensations in the mammary glands, even against the background of their swelling usually does not occur. Many women even note that their breasts have already stopped hurting during this period.
Doctors during this period recommend the expectant mother to monitor the state of the mammary glands. Proper cosmetic care will help to further reduce the number of "stretch marks", as well as preserve the tone of delicate skin.
For this, experts recommend that you carefully select underwear. The correct bra will help the expectant mother to reduce the possibility of adverse symptoms in the future. It is very important that it is chosen correctly and not tightly squeezing the chest area.. It is necessary to choose the products sewed mainly from natural fabrics.
During pregnancy it is also very important to monitor the integrity of the skin in the area of the mammary glands and especially the nipples. Stretching and breast augmentation can cause the skin to become more dry and may crack. If such a manifestation begins to bother the future mother, she should choose a cosmetic product for the treatment of the skin. Give preference to hypoallergenic products.
Sensations
In the initial period of carrying a baby, a pregnant woman has multiple clinical signs. Carrying a baby is a truly unique biological event, and the symptoms that the expectant mother feels during her first pregnancy will never be equivalent to those that appear during the second and subsequent pregnancies.
In some cases, the future mom may have diarrhea, accompanied by high body temperature and abdominal pain. Such adverse clinical signs can be a manifestation of foodborne toxicoinfection. In this case, it is extremely dangerous to self-treat and you should immediately seek medical help.. Food poisoning is not only a dangerous condition for the most pregnant woman, but also for the baby.
Emotions and mood
Changes in the hormonal background contribute to the fact that future mothers may react too “violently” to events in life. Often this is accompanied by specific mood swings. Such changes in emotions develop in most cases fairly quickly. So, a woman can rejoice and laugh, and after a while fall into a dull mood or cry a lot.
Such changes in mental behavior are not characteristic of all expectant mothers: their appearance is largely influenced by the individual characteristics of the psyche.
Most women who have already become mothers say that it was very difficult for them to control such “flashes” of emotions during the carrying of babies. Some even noted that uncontrolled emotional response remained with them throughout the entire period of pregnancy. Other women, on the contrary, did not develop similar symptoms or were only slightly expressed.
Stress and excessive mental activity contribute to the fact that a woman begins to feel that she has a headache. Constriction of the blood vessels (spasm) leads to the development of this adverse symptom.
Strong stress also contributes to the fact that some women may experience dizziness. As a rule, this symptom appears brighter after changing the position of the body.If a pregnant woman has severe dizziness and general weakness, then she should definitely tell her doctor about these sensations.
Most often, women complain to their doctors that they have problems with sleep and insomnia. The lack of a full night rest usually contributes to the fact that the expectant mother has daytime sleepiness.
Some women at this period of childbearing may feel very tired, and as the baby grows, this symptom can only intensify.
In most cases at this stage of pregnancy, it manifests itself even when making moderate loads. A future mom can get very tired when she is doing her usual household chores. Tolerance to physical training with the development of pregnancy will decrease.
In order for a pregnant woman to be less tired, she should follow all the recommendations of doctors to maintain a healthy day regimen. If possible, reduce all possible stresses.
Exercise should also be selected individually. An excellent option to enhance women's health and psyche at this stage of pregnancy are special breathing exercises. These techniques help restore full blood oxygen supply, thereby reducing spasms of blood vessels. It promotes good functioning of the brain, as well as all internal organs.
Excessive stress can lead to the resumption of adverse symptoms. Rest, on the contrary, contributes to the restoration of nerve cells and is necessary for the physiological work of the nervous system. Proper alternation of work and rest will help the expectant mother feel much better.
A pregnant woman must remember that when she is carrying a baby, she is responsible not only for her health, but also for her baby. Mother's day regimen has a tremendous impact on the intrauterine development of the child: the calmer and more satisfied the mother, the better and more fully her baby develops.
Changes in the functioning of the gastrointestinal tract
During pregnancy, the future mother's digestive system begins to work in an unusual mode, which is promoted by the changing hormonal background.
The range of different sensations can be quite large. Unfortunately, many expectant mothers face many adverse symptoms in the gastrointestinal tract.
The most common of them, perhaps, is the appearance of nausea. Toxicosis of the first half of pregnancy, unfortunately, is now registered quite often.
No less uncomfortable symptom is vomiting. Both of these clinical signs, as a rule, develop together: intolerable and increasing nausea usually ends with vomiting.
These symptoms appear, as a rule, in the morning and contribute to loss of appetite. Some women use various tricks to get rid of nausea and vomiting: they often use citrus or mints. However, coping with the symptoms of toxemia is quite difficult.
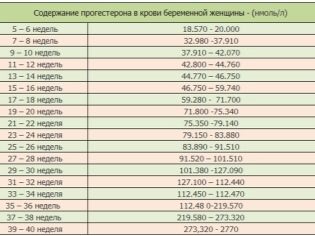
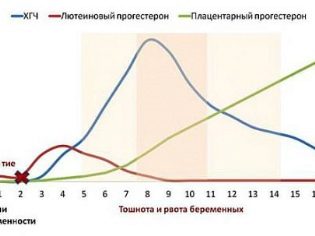
An increase in the blood of a special female hormone, progesterone, leads to the appearance of these uncomfortable symptoms. Also enhances the adverse effects and placental lactogen. This hormonal substance actively begins to produce placental tissue.
The combination of these hormones contributes to the fact that the tone of smooth muscle fibers that form the internal organs of the gastrointestinal tract changes. In most cases these adverse events are almost completely by the middle of pregnancywhen the hormonal female background undergoes further changes.
No less characteristic symptom occurring at this stage of pregnancy is the appearance of heartburn. Very often, it develops after taking fatty and fried foods.
However, in some cases, it can appear independently: for example, a high concentration of progesterone in the blood is a common cause. The weakening of the tone of the esophagus and the stomach can provoke reflux (reverse throwing) of acidic contents. This contributes to the fact that women have discomfort.
The risk of developing adverse symptoms on the part of the digestive tract organs is significantly higher in expectant mothers suffering from chronic diseases of the digestive system. In this case, the observance of proper nutrition will help reduce the manifestation of heartburn. All products that increase the acidity of gastric juice, at this stage of pregnancy, it is better to exclude.
At this time, women often experience functional disorders of the stool in the form of constipation, when the expectant mother does not defecate regularly or may even have difficulty and pain when straining.
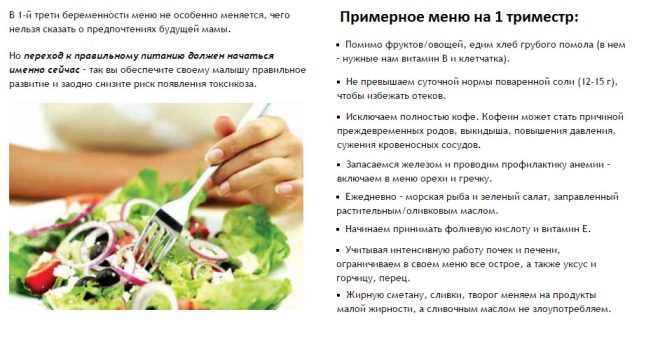
Help to normalize the regularity of the stool may correct the diet. For this it is very important to include vegetables rich in fiber in your daily diet. Fruits and berries collected in season also contain a huge amount of vitamins and microelements that are useful during pregnancy.
Lacto- and bifidobacteria are necessary for regular stools. They are involved in maintaining the normal amount of beneficial microorganisms found in the intestines. Thanks to them, the process of digestion.
The content of lacto-and bifidobacteria is high in fermented milk products; they should be eaten by the expectant mother daily. Calcium is also contained in these products, which supports the optimal functioning of the musculoskeletal system.
What worries a future mother?
Even with a healthy pregnancy, a woman can have very significant changes in her body. This contributes to the fact that she may feel a certain discomfort.
Many of the manifestations that occur are temporary. In a few weeks, as hormonal changes change, they will also transform and gradually disappear.
In addition to the natural changes characteristic of this period of pregnancy, a woman may develop some pathologies. Only a doctor can install them in time. The future mother should only be very careful to follow the changes in her body. The appearance of alarming symptoms should be a reason for her to see a doctor. Timely diagnosis helps to prevent dangerous pathology and for the fetus.
Pain in the spine
Quite often, the future mommy feels that she has a pain or pulls the lower back. This symptom usually intensifies after weight lifting or after a quick walk.
As the pregnancy develops, the pain in the lumbar spine, as a rule, only increases. This is facilitated by the increasing in size of the uterus and the rather large size of the baby. In pregnant women after IVF and carrying twins, this symptom appears, as a rule, more clearly.
The large size of the fetus is also a triggering cause of pain in the lower back. In order to reduce the manifestations of pain, many women try to take a special functional position: they sit in a sofa or chair, putting a few pillows under the lower back, and then deflect to its back. This situation somewhat "unloads" the painful part of the spine, improving well-being.
At this stage of pregnancy, the expectant mother may also note that her tailbone hurts. The actively growing uterus also leads to the appearance of this symptom: it puts pressure on the lumbosacral spine, which can lead to the appearance of pain in it.
Women with osteoarthritis or spinal fractures may experience more intense pain. In this case, they should always consult with a doctor.The doctor should consider wearing assistive orthopedic products. Special corsets and bandages reduce the manifestations of pain in the back, but these orthopedic items are prescribed for medical reasons.
To prevent the appearance of adverse symptoms in the spine of the expectant mother is very important to observe the correct mode of the day.
During pregnancy should be limited to intensive exercise, as well as not to lift heavy objects. Improper static and dynamic load can lead to painful changes in the spine, worsening the well-being of a pregnant woman.
Propensity to catarrhal diseases
The functioning of immunity during the carrying of the baby in women begins to change. This biological feature is programmed by nature. It is necessary so that the mother’s immune system does not perceive the child as a “foreign” genetic object, and therefore does not discard it.
The reduced work of the immune system leads to the fact that the expectant mother's susceptibility to various viral and bacterial infections increases. The risk of cold also increases many times.
Colds are accompanied by fever, a violation of nasal breathing, nasal congestion, runny nose. The woman begins to feel that she has a sore throat and redness.
In some cases, there is soreness in the oropharynx and even a cough. If the inflammation drops below, then pain occurs when swallowing. A woman feels unwell, increases weakness.
Future mothers suffering from chronic diseases of the upper respiratory tract are at increased risk for developing colds. As a rule, even hypothermia may lead to the exacerbation of pathology in them. At the same time, the inflammatory signs of a cold manifest themselves by the end of the first day from the moment the woman became ill.
The future mother should always be careful not to get cold or possible cold during pregnancy. It is important to remember that during this period she is responsible not only for herself, but also for her child.
Consequences of acute respiratory viral infections in the early stages of pregnancy can be quite dangerous: at this time in the children's organism, all vital organs and systems are laid.
Some viruses are able to penetrate the hemato-placental barrier, reaching the blood flow of the baby. This may contribute to the development of dangerous diseases in the child in the future, as well as aggravate the further course of pregnancy.
The severity of adverse symptoms may vary. It largely depends on the initial state of the woman. The presence of chronic pathologies of upper respiratory tract, as a rule, significantly worsens the course of respiratory disease.
Doctors do not recommend treating a viral or bacterial infection on their own. It is also extremely dangerous in the early stages of pregnancy to use various antibacterial agents uncontrollably.
It is important to remember that only specialists assign antibiotics to pregnant women. Independent uncontrolled use of these drugs can trigger the development of a child of various defects and fetal developmental defects.
If the future mommy has symptoms of a viral or bacterial infection, she should definitely consult a doctor. If the general condition does not allow, then you can call the doctor to the house. You should not go to the clinic yourself if the woman has a high body temperature.
To eliminate the adverse symptoms of viral intoxication, the doctor will definitely recommend a sufficient warm drink. Fruit and berry fruit drinks made from berries and fruits rich in vitamin C are suitable for this. Tea with lemon is also suitable as a warming drink.
For symptomatic treatment, experts use drugs that do not adversely affect the embryo. Selection of therapy should be carried out by the attending physician.
If the future mother has any allergic pathologies or intolerance to a certain type of medication, then she must warn her doctor about this - the specialist will select the optimal treatment regimen that will be effective for the sick mother, and will not harm the child developing in her tummy .
What could be vaginal discharge?
In this period of childbearing a pregnant woman may receive biological fluid from the vagina. Both physiological and pathological causal effects can cause this symptom.
Many expectant mothers may have light discharge or mucus from the vagina, looking like a clear or whitish liquid.
The consistency of the discharge is different. In most cases, it is quite liquid and has a neutral odor. The development of such clinical manifestations contribute to the special changes that begin to occur in the female reproductive system. Run their hormones.
The appearance of this type of vaginal discharge during the first half of pregnancy has a physiological nature: the effect of hormonal substances on epithelial cells leads to the fact that they synthesize glycogen, which provokes the growth of beneficial microbes that normally live in the vagina.
Such microorganisms help to maintain the optimum pH of the vaginal environment, thereby helping to protect the female body from various diseases. Changes in microflora can be the starting cause of the development of many pathologies, including thrush.
This disease is caused by the excessive development of Candida yeast fungi, the rapid growth of which leads to the appearance of uncomfortable symptoms.
An important clinical sign of the disease - the appearance of white vaginal discharge, resembling cottage cheese in appearance. Not less unfavorable symptom, complementing the appearance of discharge, is itching in the intimate zone. It can be expressed in different ways and sometimes becomes so unbearable and strong that it essentially violates the woman’s usual lifestyle.
If a woman has unfavorable symptoms of candidiasis, she should not hesitate to contact a doctor. The specialist will make the necessary treatment complex for the patient.
In the first half of pregnancy, when the process of organogenesis in the baby is actively taking place, doctors give their preference in the treatment of candidiasis to the means of local therapy. Such drugs normalize the pH of the intimate zone and reduce the inflammatory process. Proper therapy will help eliminate the adverse symptoms of thrush without harming a small embryo.
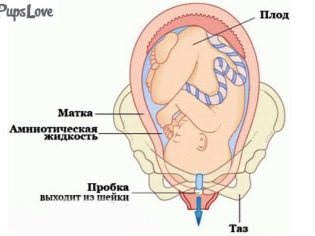
At this stage of pregnancy, the expectant mother has a mucus plug, which protects the internal cavity of the uterus from penetration of dangerous infections and exposure to external factors. It will remain in the genital tract almost until the baby is born.
The color of the discharge in early pregnancy can be very diverse. One of the worrying symptoms is the appearance of a "daub" from the genital tract. Usually, the discharge in this case has a light brown or dark color.
The appearance of such a discharge should be an occasion for consultation with the attending physician, especially if it is accompanied by the appearance in the future mother of pain in the lower abdomen or deterioration of health.
Spotting is a symptom that necessarily requires medical interpretation. Some women detect blood in their underwear after having sex or on the first day after performing a diagnostic transvaginal ultrasound. In this case, do not panic. All adverse symptoms will disappear on their own in 1-2 days.
If the bleeding from the genital tract occurred for no apparent reason, then the expectant mother should always contact your obstetrician-gynecologist. This symptom can be caused by various pathologies of the reproductive organs. Thus, a hematoma of the uterus or pathology of the placenta may be accompanied by the appearance of blood, in which case urgent medical intervention is required.
When bleeding occurs, it is very important to conduct a comprehensive assessment of the condition of both the woman and her baby. To do this, the doctor will necessarily conduct a clinical examination, and if necessary, recommend to undergo an unscheduled ultrasound.
These studies are necessary for the doctor to understand how the baby feels in the womb. Of course, to follow the discharge from the genital tract should all women.
Especially attentive should be future mothers who have a burdened gynecological history. So, if a woman’s previous pregnancies ended in spontaneous miscarriages, then she should be more attentive to her health.
Abdominal discomfort
By this time of pregnancy, future mothers may have different feelings. They are mainly due to the fact that there is an active enlargement of the uterus.
At this stage of pregnancy, it continues to increase. Its dimensions are comparable to grapefruit. Gradually the uterine walls begin to thicken. This is necessary so that the baby is reliably protected from the effects of adverse environmental factors.
Actively increasing uterus contributes to the fact that a woman has a different sensation in the abdomen: she can feel tingling or pulling pain. Usually these symptoms do not appear much.
An increase in the abdomen contributes to the fact that a woman chooses more comfortable postures for sleep. So, it becomes uncomfortable to sleep on her stomach. Even if during sleep a woman fell into this position, she should not be afraid. To harm the baby this she can not. In the future, as the abdomen increases, the expectant mother simply cannot sleep.
Discomfort symptoms that develop in the abdomen, as a rule, are not accompanied by a worsening of general well-being. During the day, they can occur several times and independently pass.
An unfavorable clinical sign is that the pain in the abdomen increases and is accompanied by the development of bleeding from the genital tract. In this case, it is important to immediately consult a doctor.
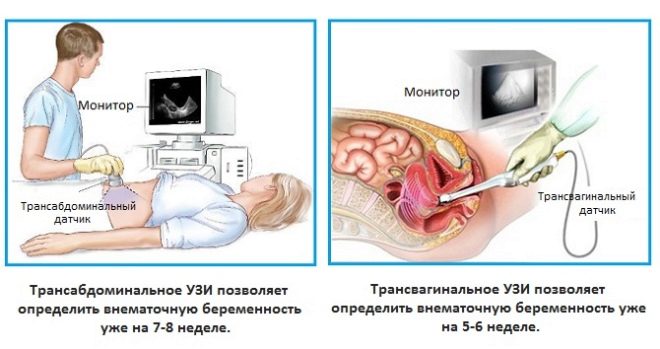
Sometimes at 7-8 weeks of pregnancy, doctors determine ectopic pregnancy. In this case, the embryo develops not in the uterus, but in the fallopian tube. This body is not provided by nature for carrying a baby.
Tubal pregnancy has no further development. This leads to its spontaneous interruption. This condition is accompanied by the appearance of heavy bleeding from the genital tract and severe pain in the abdomen. The severity of pain can be so severe that a woman can even lose consciousness.
Abdominal pain in a tubal pregnancy can also "give" in the lower back. In this case, changing the position of the body does not bring the expectant mother relief of the condition, and the symptoms are only progressing. In this situation, urgent medical intervention is required.
One of the most important clinical criteria is the determination of uterine tone. It shows how well-functioning and well-functioning the walls of the uterus are. Normally, the muscular layer of the reproductive organ (myometrium) is able to contract. This feature is due to the structure: it is formed by smooth muscle fibers located in different directions.
These contractile elements can swell under the influence of hormones, which is necessary to increase the thickness of the uterus wall. Contractility is assessed by determining the tonus.
The increase in this indicator is called hypertonus. In this state, the threat of spontaneous abortion is quite large. In this case, individual recommendations are made for the woman, aimed at normalizing the tone of the uterus.
The most optimal clinical condition - normal tonus, which is characterized by normal intrauterine pressure and at which the child is in it, develops optimally.
What surveys are conducted?
If for some reason the expectant mother did not register with the antenatal clinic for pregnancy, then she should definitely do it. Equally important is the choice of a doctor who will observe a woman during the entire period of the baby's birth.
When registering the doctor must necessarily carry out a complex of diagnostics. It is necessary in order to identify the presence of all diseases in expectant mothers. In the future, such a diagnosis will help make a possible forecast of pregnancy, as well as timely monitor the likely complications.
If a pregnant woman has any diseases of the internal organs, the doctor may refer her for auxiliary consultations to specialists of other specialties. It is better that doctors make their recommendations already at an early stage of pregnancy.
At 7-8 weeks, the doctor may recommend an ultrasound examination. It is performed for women to confirm pregnancy and exclude her ectopic variant.
Ultrasound imaging at this time can be carried out in cases of suspected multiple pregnancy, as well as women who are in high-risk groups. An ultrasound examination in this period can be shown to expectant mothers over 35 or younger than 18.
In some cases, ultrasound is performed on women who have had complex pathologies in previous pregnancies. Some diseases of the female genital organs can also become an indication for this method of research.
Ultrasound can be carried out by various methods. In most cases, doctors use the transvaginal method in the early stages. This method allows to obtain more accurate and reliable results.
There are certain medical contraindications for conducting this type of research. If they were identified, the transvaginal method will be replaced by the transabdominal. In this case, the doctor conducts a study using an ultrasound sensor, which leads the anterior abdominal wall.
To perform an ultrasound should select an experienced and qualified doctor.
Doctors say that the calmer the pregnant woman during the study, the easier it is performed. All experiences of the future mother are transferred to her baby. It is important to remember this from the very first weeks of pregnancy.
Changes in the hormonal status can be assessed by testing. One such test is the determination of hCG.
This specific hormone rises after fertilization. Its concentration in the first half of pregnancy gradually increases, which is necessary for the full fetal development of the baby.
Each period of pregnancy is accompanied by specific changes in the concentration of hCG. So, at week 8, the rate of this hormone in the bloodstream is approximately 80000 mIU / ml.
This clinical criterion is averaged. The future mother should not immediately panic if for some reason he deviates from the norm. In this case, you should definitely consult with your obstetrician-gynecologist.
If a woman bears several children at once, then her hCG levels will differ. In this case, the doctors use special tables with chorionic gonadotropin norms, compiled for multiple pregnancies.
A future mother, who is registered at the antenatal clinic for pregnancy, will definitely be assigned other tests. So, it must necessarily pass a general analysis of blood and urine, as well as biochemical research.Also determined blood sugar, RW, hepatitis B, HIV.
In some cases, the complex of analyzes can be expanded. This mainly occurs when a pregnant woman has any chronic diseases of internal organs. In such a situation, recommendations for additional diagnostics are made by doctors on the appropriate profile of pathologies.
Is it possible to have a sex life?
This question is quite common. It often happens that couples, fearing to harm their future babies, consciously limit sex.
Doctors say that future parents should choose more comfortable postures so that the woman does not feel any discomfort or pain in the abdomen.
Conducting sexual life is possible with a healthy course of pregnancy. If the risk of developing pathologies is rather high, the doctor may advise on the need to limit sex.
It is important to note that each specific situation is individual. The possibility of conducting a sexual life with safety for a baby is determined only by an obstetrician-gynecologist, who observes the expectant mother and knows about the peculiarities of her health.
Features of embryonic development
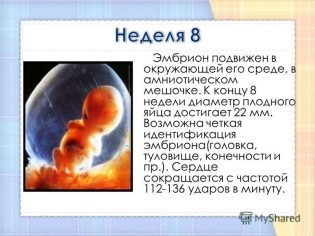
During this gestation period, the doctors call the baby the “embryo”. Its dimensions are so small that they are accurately determined only when conducting ultrasound.
This period of pregnancy is very important. The baby forms important organs and systems. As such a bookmark will occur, so in the future the child’s body will function after birth.
The size of the embryo is quite small: it is 1.5 cm in length and weighs very little - about a couple of grams.
Scientists note that in the first 8 weeks of embryonic development, a child has a huge leap in physiological development. Such changes in the future after the birth of the baby and will not occur.
In addition to the body of the child, the internal organs begin to actively form. So, liver tissue and kidneys appear.
Interestingly, the crumbs have already formed a real heart that functions. Baby's heartbeat is an important clinical sign. This indicator is evaluated during the ultrasound. To do this, the specialist calculates the number of heartbeats for 60 seconds.
If the embryo's heart beats too often, doctors diagnose it. tachycardia. The decrease in the number of heartbeats for a set time is called bradycardia.
The number of beats of a small heart within the normal range (110-130 beats per minute) indicates that the baby’s cardiovascular system is working optimally. It is very important to monitor the heartbeat of the embryo, since a change in this clinical indicator is a sign of dangerous intrauterine pathologies.
At this stage, the child continues laying the digestive, respiratory and reproductive systems. To determine the sex of the baby by ultrasound can be a little later, as the reproductive organs are only laid.
What does an embryo look like?
At this early stage of pregnancy, a small embryo resembles a tiny person and has an elongated body.
The face of the baby at this stage of embryonic development begins to change, his eyes begin to be laid. They even have the first beginnings of the retina and color pigment. The eyes on this term in a child seem huge, which is facilitated by the absence of eyelids. Orbits also continue to form.
The nose gets a clearer contour, but it is still flat. Gums and even the beginnings of milk teeth form in the oral cavity. Gradually begin to form ears. First hands of small fingers appear on hands and feet. However, they are still adhered to each other. In the future, they will be separated.
For more information on the 8th week of pregnancy, see the following video.