11 week of pregnancy: what happens to the fetus and the expectant mother?
The first, most difficult trimester of pregnancy will soon come to an end. Week 11 is one of the final stages at this stage. During these periods, a very important first prenatal examination is waiting for the woman.
How many months is it
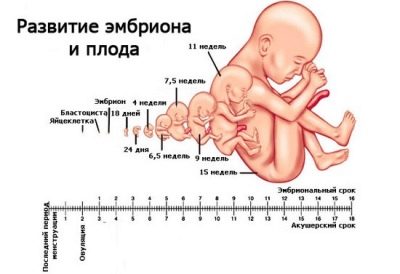
Speaking about the 11th week of pregnancy, it means six days in the interval between 10-11 weeks. 11th in a row she is in the understanding of doctors. An obstetric period is always two weeks longer than the actual one, since the countdown is from the first day of the last menstrual period. The obstetric month is exactly 4 weeks, and the whole pregnancy is 40 obstetric weeks.
Now it is 11 weeks, which means that the 9th week has already passed from conception.
That is how much time the baby develops inside the mother's womb. Week 11 is the second last term in the first trimester, and within two weeks the woman will enter the second third of the baby's term. Since the delay of menstruation, which became the main symptom of the onset of pregnancy, 7 weeks have passed.
9 embryonic week (or 11 obstetric) is the third calendar month. So that with doctors, with whom the woman has yet to communicate for quite a long time, there are no misunderstandings about the timing, it is better to get used to obstetric standards, because all tests and studies are oriented towards the norms for obstetric weeks. Having told the doctor now that you have the ninth week of pregnancy, you will mislead him, because by medical standards, she is already the eleventh.
Baby development
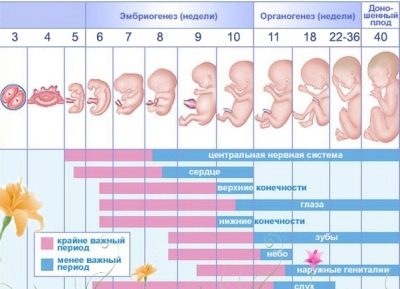
The period of the formation of internal organs left behind. The baby now has all the organs, and the task of the coming weeks is to debug their work and interaction. The baby stopped being an embryo last week. His tail disappeared, and the usual human tail bone appeared. He is the fruit and will remain so until the very birth.
The most dangerous period, from the point of view of an error in the laying of organs and the death of a baby due to negative external and internal factors, was left behind, but the threat was not completely over. A woman should be extremely careful. You can breathe freely when the second trimester begins. - “golden” time of gestation. For 9 weeks of development in my mother's tummy, the baby has achieved great success.
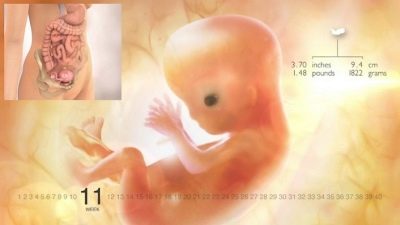
Height and weight
The baby does not grow as fast as it did during the embryonic period of its development, but the growth is constant, every minute and rather intense. Soon the crumb will slow down even more and begin to gain weight, but for now the arms and legs are growing pretty quickly. The growth of crumbs from crown to heels this week averages from 5 to 7 cm. The weight of his body is from 9 to 15 grams.
To imagine what size the child has reached, it suffices to recall what a pear looks like in small sizes.
Nervous system
Departments of the nervous system are formed, but they will have to develop actively throughout the entire pregnancy and even after the birth of the baby. The brain of the baby has two hemispheres, the cerebellum and the medulla. All departments of this "control center" are in their places.
Every day at week 11, the number of medulla cells is rapidly growing: about 250 thousand cells per day. This week, there are some well-established reflex neural connections. Every hour between the cells of the nervous system of the baby several new ways of communication are established. The brain can not yet control all the processes that occur in a small body, but he is already trying very hard to cope with this.
At the 11th obstetric week of pregnancy in the child, the central and peripheral nervous systems are clearly distinguished. The cerebellum begins to work, but for the time being it is impossible to achieve the coordination of movements, which it must ensure - the time has not come yet. It is at week 11 that the baby masters the grasping reflex, and now he can touch himself, the umbilical cord, and the list of fetal intrauterine “entertainments” expands.
At week 11, the crumb's nervous system begins to provide its response to external stimuli. Now he can feel mother's cough or strong shaking if mom drives a car over large bumps. Around the end of this week, the taste buds in the mouth begin to work, and the baby begins to distinguish the taste of amniotic fluid.
Internal organs
Organogenesis is completed by about 95%, which means that the internal organs are formed. This week continues their growth and development. As they grow, the organs master new functions, and very soon they will begin to work in the “adult” mode.
The heart of a child has four chambers, which is easily determined on ultrasound as a four-chamber slice. It beats confidently and rhythmically. Heart rate at week 11 is an average of 165 beats per minute. The normal range is considered to be a heartbeat from 153 to 177 beats per minute.
Through the blood vessels, the formation of which is almost complete, the blood pushed out by the heart goes to all organs. The vessels of the placenta also begin to work in full force, now with their help the baby receives vitamins, useful substances, minerals, oxygen from the mother’s blood and gives back to the mother the products of his metabolism, and they are taken out by the mother’s kidneys.
At week 11, the liver grows most actively. Its weight is now as much as 10% of the total mass of the fetus. Liver cells divide rapidly, because in the very near future, this organ will have to assume important functions in order to ensure the further development of the child.
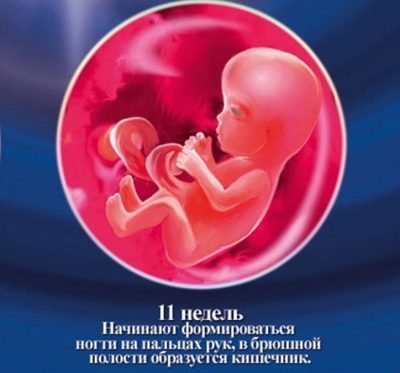
The formation of the digestive organs continues: this week the intestine “learns” to peristalsis, starting gradually to decrease. The kidneys produce and accumulate urine, the bladder is emptied once an hour.
All the fluid secreted by the child enters the amniotic fluid, but this fact should not cause concern to the expectant mother - amniotic membranes update the composition of water approximately once every 3 hours. The environment therefore remains sterile and safe for the baby. The pancreas produces insulin, which is necessary for the breakdown of carbohydrates, and the thyroid gland begins to produce thyroid-stimulating hormones.
Appearance
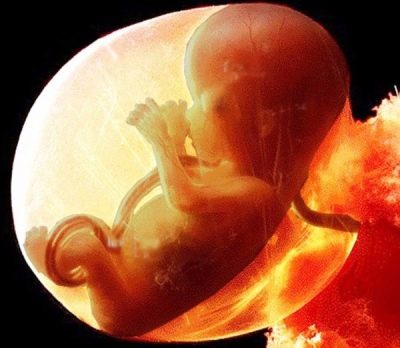
The head is still the largest part of the body, now it is about half of all proportions. However, it has already acquired a completely human rounded shape. For the sake of justice, it should be noted that with proportions now everything is not the best way, not only with respect to the big head, but also the limbs. The pens of the baby are longer than the legs, all limbs look shorter than necessary, but this is a temporary phenomenon. Every day the image of the child acquires more and more human features.
The eyes, which were previously on the sides of the head, move to both sides of the nose by the 11th week, occupying the position they were supposed to have. At this time, the retina is forming, the iris is laid, the lens and the cornea grow. There are already visible lips and nose on the face, there are small ears that grow, and soon the baby will be able to hear. On the head grow hair. The abdomen and chest are separated by a diaphragm.
The child has a neck, shoulders and forearms are highlighted, the “shoulder blades” at the end of the arms and legs are divided into fingers. This week, the baby begins to squeeze them into cams, trying to touch himself with his fingers, grabbing the umbilical cord, if he "falls on the arm."
The child’s bone tissue is growing intensively, therefore, right now, a woman should provide the baby with calcium to the maximum.
The baby's skin becomes more sensitive due to the development of nerve endings, but it still remains very thin, almost transparent, through which the entire circulatory network is visible.
Floor
The sex glands begin to produce sex hormones: boys now have their testosterone, and girls - estrogens. External genitals begin to form from the genital tubercles that now exist between the legs. While the bumps in boys and girls look almost the same, it's almost impossible to catch the difference. But by the end of 11 weeks, the bumps of the boys begin to lengthen, turning into a penis, and the maiden hillocks - to decrease and turn into the labia.
These changes are so microscopically so far that it is almost impossible to examine them on ultrasound, although sometimes there are doctors with rich professional experience who, by the appearance of the sexual tubercle at week 11 and the angle of its inclination, intuitively guess the sex of the child.
Of course, no one gives guarantees. With great precision, we can speak of the field only after the external organs are fully formed. This usually occurs by 15-16 weeks of pregnancy or a little later. In the meantime, with the question of determining the sex of the doctor on the ultrasound is better not to stick - the probability of error is too great, and none of the doctors wants to be wrong.
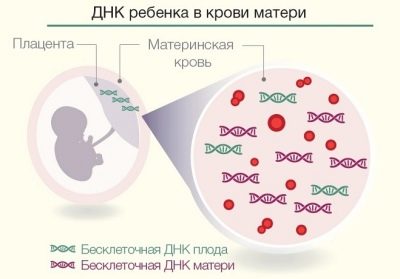
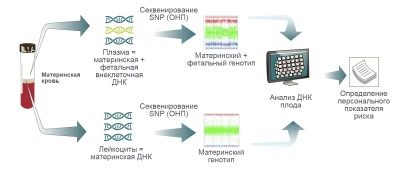
It is possible to find out the sex exactly at this time only with the help of a non-invasive prenatal DNA test, which allows you to isolate the baby's red blood cells from the mother's venous blood sample. They get into it from about 8 weeks of pregnancy. From the red blood cells, crumbs produce DNA, which gives a complete and unquestionable answer to the question about the state of health and sex of the fetus. Such a study is worth tens of thousands of rubles; it is not done at every clinic, but only at medical genetic centers.
After weighing all the pros and cons, a more reasonable solution would be to wait a few more weeks and find out about the gender of the child on time.
What can do baby?
Starting from 10-11 weeks, the baby will acquire new skills weekly. His brain, nervous system and body changes. Already, the baby is sleeping and awake. In moments of wakefulness, he actively entertains himself, trying to explore the world around: touches his face, brings his hands to his mouth, and soon he will learn to suck his fingers. At week 11, the baby begins to move more actively.
Now he knows how to make swimming movements with his feet and arms: with his legs he scoops when moving, and if the feet touch the wall of the uterus, the crumb is reflexively repelled from them in the opposite direction.
At week 11, the baby drinks and “inhales” the amniotic fluid, they may or may not like their taste. The baby opens the mouth not only to take another sip of amniotic fluid. Surprisingly, this week the little child learns to yawn. And the crumb will often do this, since such movements help the development of facial muscles, jaws, and respiratory organs.
Mother still does not feel all the active movements and movements of the baby - the size of the crumbs allow him to move freely in the uterus, almost without touching its walls. Touches are light, almost imperceptible. The movements will be felt later, when the baby is older.
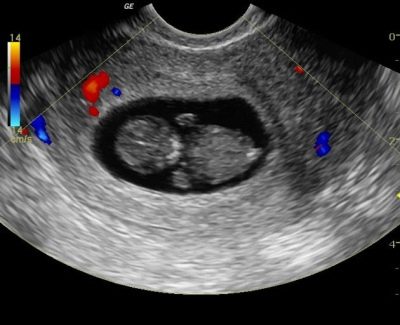
Baby on ultrasound
An ultrasound scan this week may be part of the first prenatal screen if the doctor deems it necessary to schedule it now. Referral to screening is most often given from 11 full weeks to 13 weeks inclusive, but the methods and recommendations of the Ministry of Health do not prohibit conducting a study even at week 11, when there are 10 full weeks of pregnancy.
Ultrasound is performed transvaginally or transabdominally. What sensor to use, the doctor decides, as long as the visualization is satisfactory. On the ultrasound of the baby is already clearly visible, you can even look at the profile of his face. It is important in which part of the uterus the baby “settled”: in the upper, middle or lower. Preferred are the upper and middle position of the fetus relative to the exit from the uterus.
It is at week 11 that the gestation period is most accurately determined, with an increase in the term the accuracy will decrease. Now the gestational age of the crumbs is judged by the coccyx parietal size (CTR). In fact, it is the size from the coccyx to temechka; one should not confuse KTR with growth. The rate of this indicator is now as follows:
The kopchiko-parietal size (KTR) of the fetus at 11 obstetric pregnancy week:
The average statistical rate of KTR, mm | Permissible range, mm | What corresponds to the period of pregnancy |
33 | 28,0 — 39,2 | 10 weeks + 1 day |
35,2 | 29,5 — 40,5 | 10 weeks + 2 days |
36,7 | 31,0 — 42,5 | 10 weeks + 3 days |
38,3 | 32,5 — 44,0 | 10 weeks + 4 days |
39,9 | 34,0 — 45,6 | 10 weeks + 5 days |
41,5 | 35,5 – 47,2 | 10 weeks + 6 days |
43 | 37,0 — 49,1 | 11 weeks exactly |
On ultrasound, which is part of the screening, the so-called markers of chromosomal abnormalities are necessarily determined - the developmental characteristics of children with incurable genetic pathologies.
These markers include TVP (thickness of the collar space) and the length of the bones of the nose. In children with chromosomal abnormalities, it is often at the end of the first trimester that there is a large accumulation of fluid in the cervical skin crease, which is defined as the excess of TMA from the norm. It can also be a flat face, because the deformation of the facial bones is accompanied by almost all chromosomal syndromes and mutations.
The rate of thickness of the collar space at week 11 is 1.5 mm. There is nothing wrong if this size "fits" in the range of indicators from 0.8 mm to 2.2 mm. The bones of the nose of the baby are still less than a millimeter, they are usually not measured at week 11. It is enough that the doctor sees them in principle and indicates that they are visualized.
Other sizes on this period are estimated quite rarely. But if this happens, it will be useful to know what their norms are for this week:
- BPR - 16-18 mm;
- thigh length - 6-7 mm;
- the diameter of the chest - 19-20 mm.
The length of the handles and head circumference is not measured.
Feelings of the future mother
This week there are no women who do not feel pregnant at all. Even if there is no toxemia, it is not sickening and nauseous, now almost all women become more forgetful and scattered. This condition is popularly called “brain edema of pregnant women,” and this is not too far from the truth.
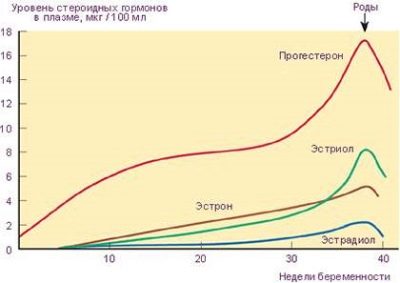
Under the action of the hormone progesterone, which from the first hours after conception is produced in the body of the future mother in large quantities, fluid accumulates in the tissues, which causes small swelling, they may not even be visible visually. The hormone acts on the brain, resulting in too strong emotions are suppressed at the hormonal level.
This is a protective mechanism designed to protect the baby from strong emotional outbursts of his mother. Absent-mindedness, drowsiness, forgetfulness are side effects from such a sedative effect. In general, a woman’s mood is becoming more stable than in previous weeks. Pregnant is not so often crying, annoyed. Most women say that they feel completely immersed in themselves, calmly contemplating all the wonderful changes in their condition.
Symptoms of toxicosis in most women may begin to recede, which is perceived as a significant long-awaited relief. However, you should not worry if toxicosis does not end in a hurry. Its manifestations up to 13-14 weeks are considered completely normal.
Hormonal restructuring is still not the best effect on health, many pregnant women this week there is insomnia: some are tormented by increased appetite, others - excessive salivation. Almost everyone has frequent urination.
A woman begins to feel truly pregnant, because it becomes more and more difficult to sleep on her stomach. From time to time, the growing uterus causes inconvenience - a woman may have complaints that the back, back pain can be caused by a sprain of the ligaments holding this organ. From time to time, tingling in the uterus, associated with the compression of the nerve plexus, can be observed.
Headaches continue to plague the pregnant woman. My head hurts because of the changed hormonal background, but gradually everything is normalized and compensated, and perhaps this week the woman will feel that her state of health has improved markedly.
Against the background of a high content of progesterone in this period, diarrhea, constipation, heartburn and increased flatulence in the intestine are not excluded. Reduce the unpleasant manifestations of the "interesting situation" will help proper nutrition. A runny nose, which appears often in the first weeks of pregnancy, should not scare the expectant mother, if there are no other symptoms: no sore throat, no cough.
Nasal congestion has a physiological nature, it is caused by swelling of the mucous membranes, which occurs under the action of pregnancy hormones. Usually in the second trimester, nasal breathing is restored.
At week 11, women who go to a screening study may be very nervous and worried about the upcoming diagnosis. Given the number of reviews, and not the most positive, the mood can be severely undermined. During this period, it is important to calm down, turn away from everything bad and believe in the best.. It is good to enlist the support of relatives and friends, to share with them your fears and fears.
If there are no such people in the environment of a pregnant woman, you can contact a psychologist who accepts absolutely free in every antenatal clinic.
Changes in the body
At 11 obstetric weeks, the intensity of all metabolic processes in the female body increases by about a quarter. This means that now calories are burned much faster, metabolism improves. Due to the fact that the placenta "started" to perform its duties, the volume of circulating blood increases. This can cause a short-term bouts of dizziness in a woman, feeling that she is thrown into a fever in the absence of an objective increase in body temperature, increased sweating, a woman is more thirsty and needs to be drunk.
The size of the uterus is more than doubled, now it is about 10% of its full volume by the end of pregnancy. The female reproductive organ fills the entire pelvic area closely, and it begins to rise above the bosom. Therefore, the woman feels some heaviness, "fullness" in the lower abdomen. The location of the uterus now affects the shape of the woman’s tummy - it rises 3-4 centimeters above the bosom, and this gives the stomach an interesting roundness, although visually the woman does not look pregnant yet.
Clothes that fit just before conception are already too small and cramped. At the waist a woman added 2-3 centimeters, her hips “sounded a little”.Slightly protruding tummy is visible only to the woman and her close people. The rest can not even guess that inside the woman is actively developing a new life. The weight of the uterus now exceeds 150 g in primiparous and is almost 300 g in the second and subsequent pregnancies.
Complaints that from time to time pulls the waist and back, can be explained by sprains and muscles due to the growth of the uterus. “Lumbago” in the perineum is also associated with the beginning exit of the uterus beyond the pelvis.
Pregnant breasts grew by about 2 sizes. At week 11, this fact pleases everyone except the most pregnant one, who, besides having to buy new underwear, is worried about pain and a feeling of distention in the mammary glands. Many inflamed mugs have darkened in women, Montgomery's hillocks appear on them, the nipples have become hypersensitive, colostrum can be released in multiparous ones.
Unpleasant sensations in the breast should end soon, because the most important stage of preparing the breast for breastfeeding falls precisely in the first trimester.
In the middle of pregnancy, the breast grows less, glandular tissue almost does not change its volume, respectively, pain, itching and aching recede.
Weight gain at week 11 is normally more than 2 kilograms for the entire period. Weight gaining is now important - the doctor will pay close attention to the number of grams added at each scheduled admission. By this date, some of the future moms come up with a minus result. This is usually observed in women who are tormented by severe toxemia, which prevents them from fully feeding.
It’s not worth worrying about, because the kilos lost in the first trimester will quickly return and turn into a gain from the top in the second trimester.
The hormone hCG, which is produced from the first hours after the fertilized egg has been attached to the uterine cavity by chorion structures, is approaching its maximum value this week. He does not have much time to grow usually after 12-13 weeks the level of gonadotropic hormone begins to gradually decline.
No pain at this time can not be considered normal, except for a small ache in the lower back, which is short-lived and unexpressed. With the appearance of any pain syndrome - whether the stomach, stomach, kidneys or other organs hurt - you should immediately consult a doctor, because now the burden on the female body is so great that exacerbation of chronic illnesses, the presence of which a woman could forget for a long time.
This week, a pregnant woman may notice some increase in secretions from the genitals. They are associated with hormonal changes. Normally, they have a light white or yellowish shade with a slight unsharp sourish smell. The appearance of blood in the discharge, blood streak, the appearance of a brown "daub" is regarded as a pathological condition. Causes of green and gray discharge with an unpleasant odor can occur in infections of the genital tract or in the purulent inflammatory process of the reproductive organs.
White discharge, resembling cottage cheese, with the smell of yeast dough may indicate the development of thrush. This unpleasant disease happens more often in the initial stages of pregnancy, when the hormones are only beginning to change, but even at week 11 thrush is not uncommon.
Analyzes and surveys
This week's tests are done as part of a screening if he is appointed now. If there is still a week or two before the prenatal examination, then only urine analysis can become mandatory - it is taken before each scheduled visit to the doctor.
If a visit to the antenatal clinic is scheduled for this week, then a few days before it is worth taking care of collecting urine and transporting it to the laboratory.
Most women are already registered at the antenatal clinic this week and most of the extensive examination that was scheduled for registration has already been completed. But the doctor may also prescribe individual examinations if he considers it necessary, for example, a blood test, if a woman complains of weakness and dizziness, or an ultrasound scan when abdominal pain and abnormal discharge from the genitals appear.
Screening
The study, which is recommended for all pregnant women in the first trimester, is designed to identify women who are at high risk for the probability of having a baby with chromosomal abnormalities. Such anomalies include Down syndrome, Turner, Patau, Edwards, Cornelia de Lange. All of them are hereditary, incurable, many, with the exception of Down syndrome, are lethal, that is, they lead to the intrauterine death of a baby or his death within a short time after birth.
The study is conducted by everyone, but women who are at risk if they can conceive such a baby especially need it:
- become pregnant after 35 years;
- having a child with chromosomal abnormalities;
- having a history of stillbirth, a few miscarriages, missed pregnancies;
- having a "complex" genetic history - one of the relatives, including relatives of the sexual partner, the husband, has hereditary diseases;
- married, become pregnant as a result of incest.
If screening is scheduled for week 11, the woman will have to do an ultrasound scan and donate blood from a vein. All this should be done in one day, so that the time difference between the studies was minimal, since neither the ultrasound results nor the laboratory data on the composition of the blood individually do not represent any value.
Only a summary assessment helps a special computer program to take into account individual risks (age, bad habits, history) to calculate the individual risk of fetal abnormalities.
Before undergoing screening for two or three days a woman should avoid fatty foods, overeating, severe stress, excessive exercise, lack of sleep. All this can affect the hormonal background. Blood is taken from a vein in the morning, you need to come to the consultation on an empty stomach. Laboratory workers use the biochemical method to determine the concentration of the hormone hCG and a special protein that appears in the blood plasma exclusively during the child's birth, PAPP-A.
A good result is considered if the content of these substances at the 11th week of gestation is in full compliance with the international standard norm: 0.5-2.0 MoM.
On ultrasound, which is carried out on the same day, they evaluate not only the overall development of the crumbs, but also markers of genetic pathologies. Thus, the absence of nasal bones on this period automatically increases the likelihood of an unfavorable prognosis, as does an increase in the rate of thickness of the neck space. The norms of these indicators are presented in this article above.
Other studies
Other tests and examinations at this time are appointed only when necessary and recommended by the doctor. If the pregnancy occurred after in vitro fertilization (IVF), a blood test for thyroid hormones, as well as the concentration of progesterone and hCG, is mandatory. If a child is conceived naturally, there is no need to study the hormonal background.
However, the first trimester can occur against the background of complications, the threat of abortion. Then the doctor is obliged to appoint an additional examination.
Possible problems
The problems that may appear this week are quite diverse. In general, the period dangerous for a child can be considered as passed, but not all problems are left behind. Some of the difficulties that a woman may face at this time are indicated below.
Risk of miscarriage
According to statistics, more than 70% of pregnant women face such a pathology of pregnancy.The shorter the gestation period, the more likely the adverse outcome. At week 11, the danger is not as great as it seems, but the signs of a possible threatening condition cannot be ignored. First of all it concerns pains and secretions. A woman must control these two factors and with alarming symptoms, you should immediately inform the attending physician.
Tranching pain may indicate a threat, in which there is an overwhelming desire to empty the intestines. Pain in the rectum is the first sign of a threatening miscarriage. The pain itself is cramping, the woman may feel that the uterus becomes stiff, the feeling of heaviness in the abdomen increases. This is how the increased tone is manifested.
Discharge with the threat of spontaneous interruption are most often bloody in nature.. Blood is different: the discharge may be pinkish or scarlet, brown or light streaked with blood. The general well-being of the future mother is deteriorating. Wait, when "everything goes by itself" can not, if you want to save the child. The treatment provided on time and prescribed correctly, in 90% of cases, allows you to avoid miscarriage, and the woman prolongs the fetus before the prescribed time and gives birth to a perfectly healthy child.
It is impossible to help only if the miscarriage began due to the fact that the fetus was not viable due to gross congenital developmental anomalies. In this case, no matter how hard the doctors try, nature "will take its own" - a pregnancy that is doomed to a "breakdown" will be interrupted. In all other cases, medicine can help.
The threat, if it is not caused by the malformations of the baby, most often occurs in women who decide to become mothers after 35 years, as well as women who suffer from inflammatory diseases of the reproductive system, have previously performed several abortions, are very nervous, working in harmful industries or excessively physically load themselves (lift weights, play professional sports, etc.).
Rarely enough, the threat of abortion occurs for the first time exactly at week 11. Most often, it occurs earlier, but it can be diagnosed only now, when a woman goes to the reception and an ultrasound on the occasion of prenatal screening. If there was no threat before this date, the probability that it will appear right now is minimal.
Fading Pregnancy
This is one of the most mysterious pathologies of pregnancy, because the reasons for which the baby, who grew and developed, suddenly stops doing so and dies, medicine and science are not fully understood. Among the most common versions are genetic pathologies, anomalies, both chromosomal and related to the inheritance of a mutated gene.
The effect of “harmful” factors is also considered - taking medications, bad habits, for example, smoking in the first trimester or systematic drinking of alcohol. Cause of death of the baby can be infections, viruses, sharp hormone jumps that can occur in women with endocrine disorders.
If this has happened before, the likelihood of a relapse is considered quite high.
Doctors, observing decades of pregnant women, brought out an interesting pattern: most often the fetus stops and stops developing at 3-4 weeks, 8-10 weeks and 16-18 weeks are dangerous. 11 week of pregnancy in the category of dangerous does not fall, but anything can happen.
For 2-4 weeks after the death, the ovum may still remain in the uterus, and the woman will not guess that the baby is no more. This week the truth may become obvious - on the ultrasound, a frozen pregnancy will be visible immediately.. Such a fetus is far behind the size of the norms for the duration of pregnancy, and there are no signs of life: the small heart does not knock, physical activity is not fixed.
Treatment in this case consists in curettage of the uterus, as well as subsequent therapy with antibiotics, and, if necessary, with hormonal preparations. Fetal tissue samples must undergo a genetic study to try to determine whether chromosomal abnormalities have caused such a sad outcome.
Symptoms and signs of a fading pregnancy may be absent if the woman herself has few signs of pregnancy. But if yesterday he was tormented by toxicosis, was sick from the smell of boiled potatoes and toothpaste, and today his chest suddenly stopped hurting, nausea disappeared, then this may be an indirect sign of a non-developing pregnancy. Accurate diagnosis will not cause difficulties for doctors, in this period missed abortion is easily diagnosed.
If the fetus froze at 8-10 weeks, then it may now appear pulling pain, bloody "daub", because the fetus begins to reject. Lack of timely assistance can cause serious inflammatory processes in the woman, severe intoxication, sepsis.
Bad Screening
If the results of the first screening at this obstetric week turn out to be unsatisfactory, the risk of having a child with severe developmental pathologies will be increased, a woman will be advised to visit a geneticist. The doctor will carefully recheck the laboratory data, and, if necessary, the ultrasound scan will be repeated, but on an apparatus of a higher, expert class.
Very often, at week 11, somnologists do not detect the bones of the nose because of their small size.
In this case, after a week on another device, the bones of the nose can be easily detected, and their size will fully correspond to the norm. A TVP that exceeds the norm does not always indicate that a child has Down syndrome or another unpleasant fact. Genetics know that most often, the diagnosis is confirmed when exceeding not up to 3 mm, but up to 8-9 or more millimeters.
Blood tests can also be affected by a variety of factors, including the individual characteristics of the female body. That is why in doubtful cases, the woman is assigned an invasive diagnosis. After 13 weeks, chorionic biopsy may be performed, and a little later, amniocentesis. In the first case, chorionic particles are taken for analysis using a long needle through a puncture in the abdominal cavity, and amniotic waters in the second case. According to the baby's DNA obtained from these samples, it becomes clear whether he has the above syndromes and pathologies.
To agree or not on such a diagnosis, only the patient decides. Before making a decision, she must be told about all possible risks associated with the procedures: the possibility of infection of the fetus and fetal membranes, miscarriage, fading of pregnancy, traumatizing the fetus mechanically, and the like.
If financial resources permit, it is possible to carry out a prenatal DNA test, which is completely safe for the baby and mother, and is not in the least inferior to invasive methods. In any case, do not panic. The disturbing screening results are not a diagnosis or a sentence.
Even a high risk of 1: 100, indicated in the conclusion, means only that out of 100 women with the same history and study results, only one will produce a sick child.
Recommendations to expectant mothers
As in the previous weeks, at 11 obstetric weeks, the general recommendations remain the same: walking in the fresh air, avoiding stressful situations, and a healthy lifestyle. To prevent complications in carrying babies will only help careful attention to their own health and control for the slightest changes in the state. The most frequently asked questions at this time require separate explanations.
Sex
In general, sex at week 11 with a normal pregnancy is not prohibited.It is even useful, because a woman who is sexually satisfied does not experience psychological discomfort, she is more confident in her feminine charm and appeal. However, now the couple will have to choose poses for intimate pleasures, because a woman already feels a certain discomfort in the lower abdomen.
At this time, the positions at which the woman is on top are not suitable; postures with deep penetration are also excluded. Sex should be neat, not rough and gentle.
If there is a threat of miscarriage, cervical insufficiency, cervical erosion, then with sexual relations it is better to wait until the special instructions of the treating doctor. With the appearance of pain, atypical for this period of discharge, it is also necessary to abandon intimate intimacy, because the orgasm causes the woman to strain the muscles of the uterus, which can cause miscarriage.
During this period, it is undesirable to use sex toys, gels and lubricants during sex, as well as to practice anal sex.
Nutrition
Rational and proper nutrition will help to avoid abnormal weight gain, which will greatly facilitate the second and third trimesters of pregnancy, childbirth and the restorative postpartum period. If the diet of a pregnant woman is not yet optimized, then now is the time to revise your eating habits and habits.
This week, the child urgently demands from women that foods high in calcium and magnesium are fresh greens, milk and dairy products, nuts, red meat, some low-fat varieties of sea fish. From fatty and fried foods, carbonated drinks, store sweet juices in boxes and sweets should be abandoned. The abundance of salt and spices is prohibited, even if there is no edema and toxicosis.
You should eat at least five times a day. Portions should not be large. The volume of the portion should correspond to the volume of the palms of the woman, folded "boat". Each meal, with the exception of the evening, should include proteins, fats and "slow" carbohydrates. Before bedtime, eating should be easy, for example, a glass of ryazhenka or kefir or homemade mashed fresh apples, cooked without sugar just before the meal.
It is important to drink a sufficient amount of liquid - at least 1.5-2 liters per day. It should be clean drinking water. Soups, fruit drinks and juices are not included in this amount.
Travel and leisure
If a journey was scheduled for week 11, then there are no restrictions, provided that the woman has no threat of severe toxemia and other complications. Especially carefully you should choose the destination point - too abrupt change of time zones or climatic zones at this time can cause significant harm to the health of the future mother. Trips associated with the flight by plane, require mandatory prior consultation with the attending physician.
If a woman does not suffer from blood pressure drops, she has no signs of threatened miscarriage, chorionic previa, there were no miscarriages earlier, and the pregnancy is good, the flight may well be resolved.
Treatment and medication
Immunity of the pregnant woman in the first trimester is somewhat depressed, reduced. This results in progesterone, which tries to prevent the mother's body from rejecting a small new organism, which is exactly half alien to the mother. That is why a woman is subject to all seasonal diseases and infections more than before pregnancy.
It is advisable to stay away from crowds of people, postpone visiting shopping centers, large events until better times. If a woman, despite the precautionary measures, is still ill, you should definitely call a doctor, even if the lady used to cope with a cold and ORVI on her own.Now, many drugs are banned, so the treatment of SARS, flu, tonsillitis and other ailments should be carried out only with the use of those tools, including folk, which the doctor will approve and allow, taking into account the fact of pregnancy.
At week 11, it is undesirable to take antibiotics, painkillers, antidepressants and anticonvulsants, as well as all drugs that affect blood clotting. It is undesirable to treat teeth with anesthesia, to drink immunomodulators.
Reviews
Reviews of future mothers about the 11th week of pregnancy are different. Some claim that they have already had toxicosis, they wanted to eat and enjoy life, others still suffer from nausea and bowel problems.
Some are only going to go to the consultation, because they believe that the registration should get up at exactly 12 weeks. This statement is erroneous, since the first application at 12 weeks is not considered early registration.
The woman will not receive the social supplement to the maternity funds due for the early setting, and the first screening will be held in a hurry. The rest of the examinations will shift in time for the period “after the screening”. Early staging allows you to identify pathologies and complications in the early stages and, accordingly, prevent their development.
About what happens at the 11th week of pregnancy, see the next video.