Causes and treatment of hematoma in early pregnancy
The presence of any features of the course of pregnancy requires a more careful approach to the pregnant woman and the baby, who is in her womb. Pathology, which can significantly complicate the pregnancy, is a hematoma, localized in the uterus. This article describes in detail the causes and treatment of this pathology during pregnancy in the early stages.
What it is?
Doctors call hematoma an accumulation of blood. When a hematoma in the uterus blood accumulates inside the reproductive organ. There are many reasons that can lead to this pathological condition.
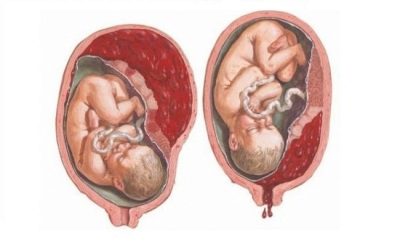
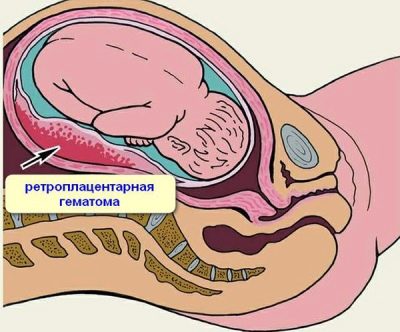
Hematomas can be different. It depends on where the blood is being poured. Retrochorial hematoma is a collection of blood in the space between the uterine wall itself and the chorion. (extra-embryonic membrane, which separates the embryo tissue from the uterus wall).
Retrochorial hematoma is an extremely unfavorable pathology. The risk of spontaneous miscarriage in this pathology is quite high. It is very important that such a hematoma be detected in a timely manner.
The formation of such a hematoma occurs in early pregnancy. This is due to the fact that the chorion is a temporary body. It is present in the body of a pregnant woman for only a few weeks, and later it is transformed into placental tissue.
The reasons
A variety of causes can lead to the development of retrochorial hematoma. Most often contribute to the development of pathology:
- dishormonal disorders;
- traumatic injuries;
- various infections;
- autoimmune diseases;
- pathologies occurring with impaired hemostasis;
- congenital abnormalities associated with anatomical defects in the structure of the uterus;
- bad habits of the mother (alcohol, smoking);
- work in harsh conditions associated with exposure to high temperatures, noise, radiation, vibration;
- associated diseases of internal organs.
The reasons that can lead to the development of retrochorial hematoma in the uterus are so numerous that it is sometimes difficult for doctors to establish only one of them. Quite often, the development of this pathology is preceded by the impact of several reasons simultaneously.
In women who have a burdened obstetric and gynecological history, the risk of retrochial hematoma in early pregnancy is quite high. If the expectant mother underwent any surgery or surgery on the uterus (curettage, removal of polyps) before the pregnancy, then in the first weeks of the baby’s birth, she may develop retrochorial hematoma.
In cases where it is impossible to establish a single cause, doctors resort to the appointment of symptomatic therapy. It is aimed at correcting the developed adverse symptoms. Such treatment should reduce the risk of developing dangerous complications, which are not uncommon in case of retrochorial hematoma.
How does it manifest itself?
The severity of adverse symptoms in a hematoma in the uterus depends on its size.Usually a large hematoma leads to the appearance of marked clinical signs in the expectant mother. Some symptoms may be so severe that they can significantly worsen the general condition of a pregnant woman. If the hematoma in the uterus is small, then the symptoms may be mild.
One of the characteristic symptoms that can develop in this pathology is appearance of discharge from the genital tract. As a rule, they have a brownish tint. If an intrauterine hematoma leads to bleeding, the discharge changes color and becomes red.
A woman with a retrochorial hematoma may also appear lower abdominal pain. Usually, pain syndrome increases after performing any exercise or after a quick walk. The rise of heavy objects can also lead to increased pain. The epicenter of pain in this pathology, as a rule, is located in the lower abdomen. However, in some cases, the pain may spread to the lumbar region or even “descend” into the hips. This irradiation (distribution) of pain is largely associated with the features of the innervation of this part of the body.
A woman who had a subchorial hematoma in the uterus in early pregnancy may experience general weakness and get tired quickly. Fatigue can occur even when doing ordinary and familiar things. Some women may experience dizziness. The expectant mother, who had a hematoma in the uterus in early pregnancy, should carefully monitor her blood pressure.
If, against the background of existing pathology, it began to decline constantly, it is imperative to notify your doctor of this. This may indicate a progression of hematoma formation. In this case, the revision of the chosen tactics of therapy and the appointment of additional drugs are required.
In obstetric practice, there are also asymptomatic cases. In this situation, a pregnant woman, as a rule, does not bother. She feels pretty good. An asymptomatic variant of hematomas in such situations is revealed, as a rule, only during an ultrasound examination. Reviews of many women with this pathology during pregnancy, this is also confirmed.
Effects
In the early stages of pregnancy, the chorion performs many different functions. A small forming organism needs this special membrane, which protects it from the effects of many external factors. Hematoma, which appears in the uterus, leads to disruption of the functioning of the chorion. This effect is reflected in the general course of fetal development.
Many pregnant women are interested in the question of whether a hematoma can self-dissolve. If it is small, then it may disappear. Usually the hematoma resolves in 2-4 weeks. In some cases, it may take more time. The prognosis of the course of pregnancy after the “disappearance” of a hematoma in the uterus is usually favorable. The future mother in this case can carry the child in the womb right up to the birth.
Hematoma of the ovum can be a very dangerous pathology. It threatens to impair the blood supply of an actively developing small organism. Lack of essential nutrients and oxygen contributes to the fact that a small embryo begins to develop poorly. Ultimately, this may contribute to the development of defects, developmental abnormalities.
Another possible complication that can develop with uterine hematoma is infection. Blood that accumulates between tissues is an excellent breeding ground for pathogens. The microorganisms that got there quickly develop, which leads to the development of inflammation.The inflammatory process that begins with such an infection, both worsens the general condition of the expectant mother, and significantly affects the embryo.
Retrochorial hematoma, which has a fairly significant size, often contributes to the detachment of the embryo from the uterine wall. In this case, pregnancy, unfortunately, ends in a spontaneous miscarriage. At the same time, the fetus "leaves" the uterus along with the blood that appears during the development of bleeding during detachment.
Spontaneous miscarriage can be very dangerous for the condition of the woman herself. It happens that the bleeding that develops after the death of the embryo and its exit from the uterus is quite abundant.
Severe blood loss can even lead to the development of hemorrhagic shock. In this condition, a woman’s blood pressure drops sharply and her consciousness is disturbed. In such a situation it is very important to immediately seek medical help. In case of severe bleeding, a woman should be hospitalized in the hospital (for intensive care).
Treatment
The main goal of therapy is to stop the growth of hematoma. In this case, all prescribed drugs should lead to the compensation of the resulting violations and the maximum preservation of pregnancy.
Recommendations on adjusting the daily routine are also made for the future mother. They, as a rule, exclude intensive physical load, weight lifting.
In this case, the expectant mother is recommended to get enough sleep on a regular basis, eat fully and not abuse visits. baths or saunas.
Drug therapy
Selection of drugs for hematoma of the uterus is carried out strictly individually. To do this, the doctor must determine the cause that led to the development of these disorders. Medicines can also be prescribed to correct any symptoms that have occurred.
Hormonal drugs
To correct the resulting violations, doctors often resort to prescribing drugs that contain analogues of female sex hormones. Usually they are appointed for a fairly long period of time. The prescription of such drugs is largely justified even at high risk of spontaneous miscarriage. Often, doctors prescribe hormonal preparations to their patients and up to 14-16 weeks of pregnancy.
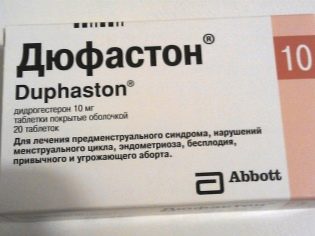
To normalize the level of the main pregnancy hormone most often used synthetic analogues of progesterone. They help to improve the hormonal balance in the body, as well as contribute to the prolongation of pregnancy until the second trimester. By this date, the placenta appears in the body of a pregnant woman, which normally synthesizes progesterone.
If the placental tissue performs its functions quite well, then the need to take synthetic progesterone drugs almost disappears. In this case, hormonal drugs can be stopped.
Often, to correct the violations that have occurred, doctors prescribe the hormonal drug Utrozhestan to expectant mothers. The active ingredient of this tool is progesterone, which is an important pregnancy hormone. When administered orally, the drug is quite well absorbed from the gastrointestinal tract. Prescribed medication obstetrician-gynecologist, who oversees the course of pregnancy.
Antispasmodics
To relieve severe pain in the abdomen, doctors resort to the appointment of antispasmodics. It is important to note that such drugs are prescribed with extreme caution. In some cases, taking antispasmodics can lead to bleeding. Prescribe antispasmodic drugs should only a doctor. Such funds are written out in short courses, on average, for 4-5 days.
During treatment with antispasmodics, a pregnant woman may have a bloody or dark colored discharge from the genital tract.So from the uterus is removed part of the blood that is there.
Antispasmodics relieve spasm of the blood vessels, which leads to the appearance of such specific secretions. When part of the blood leaves the uterus, the expectant mother may feel much better.
Preparations containing folic acid
In the early stages of pregnancy, such agents have a positive effect on DNA synthesis, which is actively occurring in the cells of the rapidly developing organism of the embryo. With insufficient intake of folic acid in the early period of organogenesis, a child may experience various pathologies and even defects in the structure of the internal organs.
Retrochorial hematoma, which appeared in the uterus in early pregnancy, is accompanied by impaired functioning of the fetus. In this case, the risk of developing dangerous pathologies increases many times. At the same time, it is possible to minimize cell damage using preparations containing folic acid.
Sedatives
These funds for this pathology have more auxiliary value. Many women, after determining the diagnosis, begin to worry much about the further course of pregnancy. Such stress is dangerous not only for the most pregnant woman, but also for the baby, who is in her stomach. To normalize well-being, doctors recommend expectant mothers to walk more in the fresh air, to learn various breathing practices, to do what they love (to be distracted in every way). However, unfortunately, these recommendations in practice do not always help.
In some cases, the woman can not escape and constantly thinks about the problem. In this situation, doctors are usually forced to resort to the appointment of sedatives. Such drugs have a calming effect on the nervous system, reducing overall anxiety. During pregnancy, herbal remedies are usually prescribed that do not harm the fetus.
The choice depends on the specific situation. It also takes into account the presence of allergy to certain plant components. Very popular drugs that are used for sedation (sedation) are products containing valerian and motherwort. Usually such herbal preparations are prescribed for several weeks.
Hospitalization in the hospital
In some cases, the treatment of hematoma, which is located in the uterus, is carried out in a hospital. A pregnant woman is in the hospital until her well-being is normalized and adverse symptoms are eliminated.
Treating retrochorial hematoma can be quite difficult. Even against the background of therapy, a pregnant woman can develop complications, one of which is the appearance of bleeding. In this situation, timely assistance of qualified doctors is very important.
After the inpatient treatment, the expectant mother is discharged home. In the future, it will be treated as an outpatient.
In case of any deterioration of health, a pregnant woman should immediately seek medical help. To tolerate and hope that all the adverse symptoms disappear on their own is not worth it. Hematoma in the uterus can be an extremely dangerous pathology.
To assess the dynamics in this pathology, you can use ultrasound. To do this, the specialist determines whether the hematoma size changes with each examination. If (despite the treatment) the hematoma continues to grow, you should definitely consult with your obstetrician-gynecologist about this. With such a negative dynamics, a change in the chosen tactics of pregnancy management is required, and in some cases, additional prescription of drugs.
On how to behave in the event of this and other causes of pregnancy, see below.