Double cord entanglement
Double entanglement with umbilical cord is a fairly common complication of pregnancy. Its essence lies in the fact that the umbilical cord twice twists around any part of the body of the fetus. Modern clinical technologies allow carrying out childbirth in this pathology in most cases without consequences for the mother or fetus. Depending on the type of entanglement and possible threats to the fetus, a mode of delivery is chosen.
What are the risks for a child whose intrauterine development proceeds with a double entanglement? Is it possible to prevent the occurrence of such a defect?
The reasons
Occur cord entanglement may in the presence of the following factors:
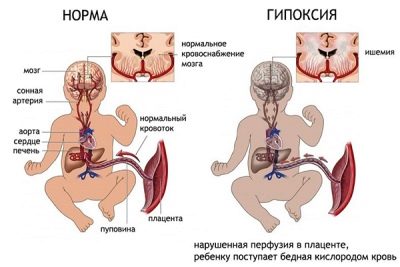
- Hypoxia of the fetus. If the fetus regularly for one reason or another experiences an oxygen deficiency, then its body can react to this with increased motor activity, because of which the baby may become entangled in the loops of its own umbilical cord and its further intrauterine development will proceed in this position.
- Increased concentration in the mother's blood adrenaline. This factor also affects the frequency of active fetal movements.
- Umbilical cord too long (more than 0.6 m).
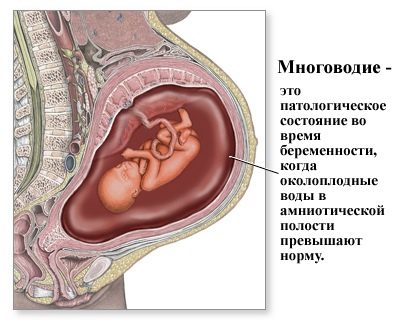
- Many water. Too much space around the baby often becomes the cause of multiple cord entanglement.
Usually, a double cord entanglement is diagnosed for 28-32 weeks, since after this period the fetus becomes large enough, which prevents its active movement in the womb.
Complications
The main danger posed by the compression of the baby’s cord by the umbilical cord is hypoxia. Also, such a complication of pregnancy can lead to the fact that during childbirth the baby will be injured. Children with a double entanglement may further suffer from periodic attacks of migraine, hypertension (persistent increase in blood pressure) or hypotension (persistent reduction in blood pressure), as well as from reduced working capacity.
Persistent hypoxia of the fetus can cause the death of a baby or lead to the development of severe neurological disorders due to the death of brain cells. This happens quite rarely and in such situations, doctors mainly prescribe delivery by caesarean section.
The effects on the body of oxygen starvation are not always manifested by obvious structural or physiological defects. In addition, the severity of brain damage during hypoxia in different children may differ: for someone, double cord entanglement is just a record in the medical record, and for someone it is a reason for permanent sitting at doctors' offices.
However, one should not think that if during childbirth the child experienced hypoxia and suffered damage in the form of any violations, then such a baby is guaranteed a disability. With the implementation of all medical recommendations, attentive care and care, such a child has every chance to grow up healthy and be no different from peers.
Diagnostics
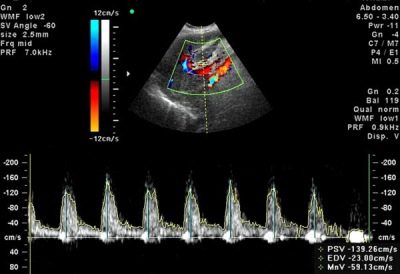
It is possible to detect the presence of double entanglement with umbilical cord using cardiotocography. The essence of this diagnostic study is the continuous recording of fetal heart rate and the degree of uterine tone. According to the indicators taken from CTG, the specialist can determine whether the oxygen starvation of the fetus.
To confirm the diagnosis, an ultrasound is performed, through which the fetus can be visualized and cord entanglement detected. Thanks to the data obtained, the doctor will be able to accurately name the number of loops wrapping around the body of the baby, and assess the nature of the entanglement - very tight, strong or not tight.
Prevention
As a preventive measure, in order to avoid the occurrence of fetal entanglement, future mother should follow a number of recommendations:
- normalize (as far as possible) your emotional background;
- walk more often and as seldom as possible be in stuffy, unventilated rooms;
- follow the basic principles of nutrition;
- timely visit the doctor, in time to pass all examinations appointed by him;
- systematically do gymnastics for pregnant women, having previously agreed on a list of exercises with your midwife.
Often, with repeated entrapment and tight compression of the baby's umbilical cord, the expectant mother is placed under observation in the hospital.
If the situation becomes threatening, the obstetrician observing the pregnancy may recommend prompt delivery before the due date.
Obstetric care
In world clinical practice, in most cases, vaginal delivery with entanglement ends successfully. If in this case neither the fetus nor the mother has any accompanying pathologies, then they are generally discharged from the maternity hospital after a few days. However, childbirth in a woman who has been diagnosed with fetal entanglement should proceed with the increased control of doctors, which includes monitoring the fetal heartbeat in the first and second stages of labor. For this purpose, methods of instrumental diagnostics are used: ultrasound, Doppler and cardiotocography.
When the baby’s head is born, the doctor removes the umbilical cord loops from his neck and the birth continues as usual. Only with a tight or multiple entanglement is the question of operative delivery. In some situations, this may be the only way to avoid generic complications.
Superstitions
Despite the progress by leaps and bounds, in our society, judging by the numerous reviews, superstitions related to various signs are still quite popular. During pregnancy, even the most sensible woman tends to succumb to prejudice. This is largely due to fear for the health of the future baby. Therefore, often pregnant women do not dare to engage in handicrafts, explaining that such actions allegedly can provoke the emergence of umbilical cord loops in the future baby.
This is due to the fact that in the old days women engaged in knitting and sewing in poorly lit huts, which were heated by a wood-burning stove, because of which the air in the house was quite suffocating. Because of this, the fetus was in a state that was not very useful for a woman for a considerable amount of time, because the mother had been sitting in a fixed posture for a long time, stooping. As a result, the baby experienced an oxygen deficiency and, as a result, began to move actively, which often caused the umbilical loops to be thrown around the neck. Noticing a similar pattern, the people composed signs that, in our time, continue to intimidate some overly impressionable pregnant women.
Today, most women have the opportunity to provide for themselves comfortable conditions for needlework. Therefore, do not deny yourself the pleasure of spending time with your favorite thing because of superstition.
There is also a belief that the entanglement of the umbilical cord is formed with frequent raising hands up. In fact, there is nothing dangerous in raising hands; in the past, women of the peasant class did hard work, raising their hands, for example, hanging wet clothes. Actions of this nature could provoke excessive activity of the fetus, which, in turn, could cause entanglement.
Our contemporaries have the opportunity to limit physical exertion to acceptable limits, so if a woman in “position” raises her hand to get a book from the shelf, her child will not be harmed by this, especially in the early weeks of gestation.
If the liftings of the hands are carried out within the framework of the fitness gymnastics, then such movements will benefit both the expectant mother and the baby.
Nowadays, when perinatal diagnosis has reached unprecedented heights, entanglement by the umbilical cord is not an extremely threatening condition for the fetus. You can avoid the development of serious pathologies due to hypoxia, subject to timely visits to a specialist and the exact implementation of all his appointments. It is also important to actively engage in the prevention of the development of such a complication.
For more information on double cord entanglement, see the following video.