What is a placental infarction and what causes it?
With the onset of pregnancy, the woman's body is rebuilt to the needs of the growing fetus and fully regulates its metabolism. The relationship between the future mother and the child is carried out using the placental barrier, limiting their vascular system. The placenta itself is a structural formation located in the uterine cavity, consisting of fetal membranes.
Many changes occur in the placenta over the course of pregnancy. It happens that the expectant mother already diagnoses a placental infarction in the later stages of gestation. The fact that this pathology is, and what is its degree of danger to the development of the fetus, will be discussed in this material.
What it is?
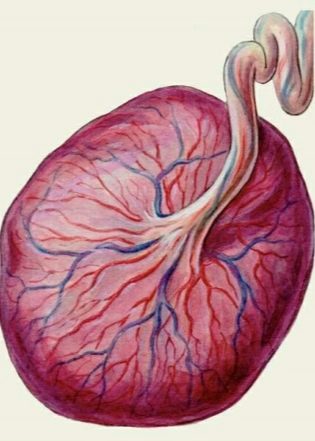
Literally from the Latin language, the placenta is translated as "flat cake". This name, apparently, is associated with the form that the body takes after the expulsion of the fetus. The placenta has a lobular structure. The lobules are separated by a kind of partitions. Each of the lobules has many small vessels. The body is designed in such a way that two isolated circulatory systems converge in it.
The umbilical cord is a cord-like formation connecting the fetus with the placenta. The venous umbilical cord vessel carries arterial blood, and in the two arterial vessels, respectively, venous flows. All of them are surrounded by a specific substance that performs a protective function. Between the systems of blood vessels of the mother and child is a barrier membrane, which is a single layer of cells. Thanks to her, the blood flows of the mother and child do not connect with each other.
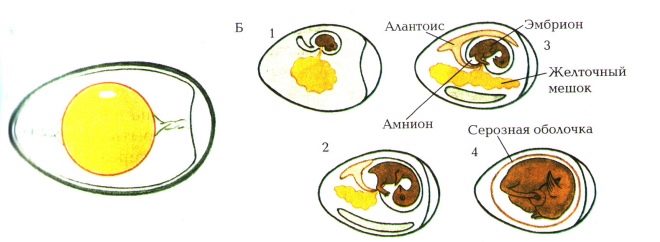
7 days after the confluence of the male and female germ cells, embryo implantation begins, that is, its introduction into the uterine mucous layer (endometrium). At this time, produced special enzymes that destroy a certain area of the mucous.
Part of the external cells of the ovum begins to form the villi. They are directed into the cavity - lacunae, appearing at the site of the disintegration of the vessels of the endometrium. The lacunas are filled with the blood of the mother, thanks to which the fetus is later fed.
Next, extra-embryonic formations are formed: chorion, amnion, and yolk sac. This process is called placentation and lasts an average of 3 to 6 weeks. These structural components of the placenta will not form tissues and organs of the child, however, its intrauterine functioning is impossible without them. The chorion will subsequently turn into a placenta, and the amnion into the bladder.
By 12 weeks, the placenta takes on a disc-shaped form, and by the 16th week, its formation is completed. As the fetus grows, an increase in the size of the placenta occurs, moreover, the density of its structure changes as the pregnancy progresses. This process is defined in obstetrics as “maturation”. It is absolutely physiological and provides full intrauterine development of the fetus.
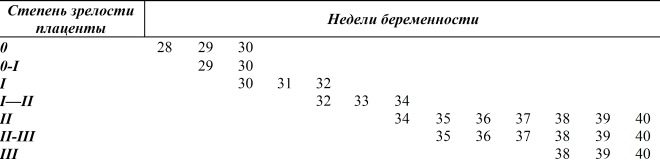
There are four degrees of maturity of the placenta:
- zero (often manifested at 30 weeks);
- the first (manifested from 27 to 36 week);
- the second (manifested from 34 to 39 week);
- the third (appears after 36 weeks).
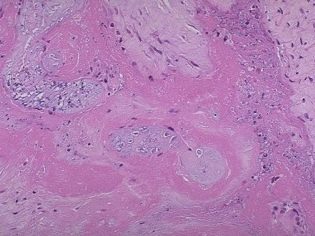
In medicine, the term "infarction" is understood necrosis (death) of a section of organic tissue due to persistent blood supply insufficiency. The placenta, like any other organ, has its own blood vessels, which supply its tissues with nutrients and oxygen, and also carry away the final products of metabolism from them.
A heart attack develops on the background of a blockage of a blood vessel and, as a result, a violation of its patency. As a result, organ tissues begin to experience acute oxygen deficiency. For a while they continue to function, getting used to another mode of metabolism. Due to this, provided that the blood flow is restored soon, the working tissue can maintain its viability.
If the reason for stopping the flow of blood in the vessel does not respond to elimination, then, after some time, the cells of the organ begin to die off and a necrosis center forms in their place. Of course, the functional ability of the organic structure in this area will be irretrievably lost.
The volume of necrotic tissue depends on the diameter and number of damaged blood vessels. Small single foci of dead tissue, formed in the first half of the gestational period, can be converted to calcinates (deposits of calcium in soft tissues) by the end of pregnancy, which is one of the manifestations of age-related changes in the placenta.
Why does it occur?
There are several pathological factors leading to the appearance of extensive placental infarctions. Most often, they are associated with certain disorders in the body of the future mother.
- Diabetes mellitus type 1 and 2. Excess glucose in the blood thinning the vascular wall, as a result of which they become fragile and brittle. As a result, hemorrhage may occur and the placenta blood supply is broken.
- Autoimmune processes. The pathological mechanism of this kind of disease lies in the fact that the cells of the immune system instead of pathogenic microorganisms begin to destroy the organic structures of their own organism. Vascular walls can also be damaged by autoantibodies.
- Arterial hypertension - persistent increase in blood pressure. Thin vessels of the placenta are damaged by high blood pressure.
- Infectious process. Once in the body of the future mother, the virus or bacteria begin to secrete toxic substances that have a destructive effect on the vascular wall.
- Thrombophilia. In this case, blood clots form in the vessels of the placenta, which can partially or completely block their lumen and cause an organ circulatory failure.
- Fat or gas embolism. Vascular occlusion occurs with particles of adipose tissue (for example, in violation of the integrity of large tubular bones) or an air bubble (usually occurs as a result of improper clinical activities).
- Toxicosis. The processes characteristic of pregnancy, can also adversely affect the circulatory system of the baby.
Symptoms
The placenta does not have pain receptors, so the infarction of the placenta does not manifest itself by subjective sensations.
Sometimes this pathological process can trigger the development of severe bleeding. If hemorrhage occurs in the central part of the placenta, a hematoma forms between it and the wall of the uterus. In this case, the woman may experience pain at the site of the pathological process.
In addition, the doctor during the preliminary examination may note the appearance of a dense formation on the anterior abdominal wall. If the bleeding has opened in the peripheral part of the placenta, then it can manifest bloody discharge from the vagina.
Danger
For the health of the expectant mother, placental infarction carries no danger. At the same time, for the fetus, the consequences of the necrosis of areas of the child's place can be severe violations of intrauterine development up to spontaneous abortion (here we are talking about extensive foci of necrosis).
From this the conclusion follows: placental infarction is a rather serious complication of pregnancy, requiring immediate treatment.
Preventing the occurrence of severe fetal abnormalities are regular examinations of women. This is especially necessary for future mothers who have a history of chronic diseases or have undergone an acute infectious process.
Placenta is an important organ for carrying and developing a healthy pregnancy. In the next video you can learn about the placenta and everything connected with it.