What threatens the short cervix during pregnancy and what to do?
The state of the female genital organs during gestation changes. If the future mother has a doctor who discovered a shortening of the cervix, the pregnancy can be complicated. This article will tell future mothers more about this common pathology.
What it is?
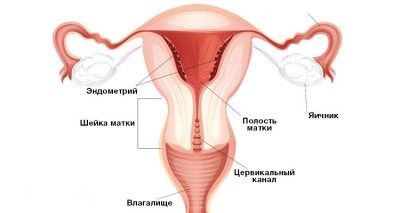
The main reproductive organ in which the baby develops is the uterus. It is located in the lower abdomen. During pregnancy, the size of the uterus varies significantly. This is necessary to ensure that the baby during childbirth freely passed through the birth canal.
A peculiar entrance to the uterine cavity is its neck. Different women have different sizes. The average length of this body is, as a rule, 3.5 cm. For most women, this size is from 3 to 5 cm.
Changing the length of the cervix is a very important clinical indicator. Doctors say that this body can be shortened to 2 cm or less. It is this pathology that is called shortening.
The cervix during the carrying of the baby changes significantly. During this period, in the female body, the uterine and then the placental blood flow increases significantly. This process contributes to the strong growth of the cervical epithelium. Such a situation in its development leads to the fact that the length of the cervix is significantly reduced.
The proliferation of epithelial cells occurs during pregnancy under the influence of various specific hormones. Estrogens contribute too much hypertrophy of the muscle layer of the uterus, which leads to a change in the tone and condition of the cervix and cervical canal.
Such a situation in many women can even lead to the development of many pathologies that may lead to the need for surgical gynecological treatment.
Causes of shortening
The narrow and short cervix is often a congenital pathology. Also, this pathological condition in the future mother may appear as a result of exposure to various traumatic actions. The cervix is shortened after an abortion, as well as other surgical interventions.
Heredity is an important feature that can contribute to the development of such a violation. In this case, similar changes occur in the mother, grandmother or sister of a pregnant woman.
In such a situation, quite often they even show similar pathologies, which were manifested during the carrying of babies. Quite often, adverse symptoms develop at 25-30 weeks of pregnancy.
To shorten the cervix can lead to significant physical exertion. It is for this reason that doctors forbid the expectant mother to engage in active sports or heavily burden her body. As an optimal physical activity, regular walks in the fresh air are suitable.
Another possible cause of this condition is the effects of various infectious diseases. Pregnancy is a period in a woman’s life, accompanied by a decrease in immunity. This condition and contributes to the fact that any pathogenic microbes can easily get on the cervix and cause inflammation there.
In order to reduce the likelihood of the development of this condition before pregnancy, a woman should always regularly visit her doctor.
The appearance on the cervix of various scars can also contribute to the shortening of this organ. These formations appear after any surgical interventions on the cervix, which are conducted by obstetricians and gynecologists.
Pathologies leading to the treatment of this organ with the help of a laser or alternative methods can also contribute to the formation of various scars on this organ.
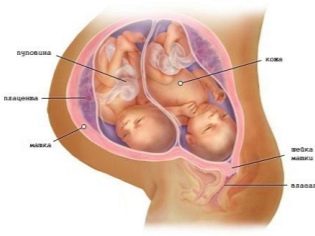
If the future mom bears a large baby or twin, the risk of shortening also increases significantly. In this case adverse symptoms progress over time.
This situation is due to the fact that the baby, developing in the womb, has a strong pressure on the cervix. Squeezing this organ leads to the fact that it significantly shortens and becomes narrower.
Pathological conditions of the placenta can also lead to the development of this pathology. One of these pathological conditions is its presentation. The large size of the placenta, which puts pressure on the cervix, causes it to squeeze, contributing to the development of shortening of the organ.
Experts identify several of the most dangerous periods during the carrying of the baby. This includes the time from 20 to 30 weeks of pregnancy. The most dangerous period for the development of this state is the 16th week.
Symptoms
During the entire period of pregnancy, a woman should carefully monitor their state of health. Adverse symptoms may appear at any time.
If the future mother has a feeling of worsening of her state of health, it is better for her to turn to her obstetrician-gynecologist unscheduled.
Quite often, adverse symptoms occur in women. 21st week of pregnancy. This period of bearing a child is very important. At this time, a woman usually begins to feel the active movements of her baby.
Many mommies' testimonies show that they feel “pushes” or “kicks” in their tummy. This condition causes them a lot of positive emotions and strongly inspires.
If, against the background of such symptoms, a pregnant woman begins to notice that she has some soreness in the lower abdomen or there is bloody discharge from the vagina, then she should necessarily and quickly contact your doctor.
31-32 weeks of pregnancy is another dangerous period of pregnancy, when a woman may have a deterioration. The most attentive for themselves at this time should be followed by expectant mothers who are carrying twins or triplets.
Women suffering from polyhydramnios are also at high risk for the development of this pathology. In order to prevent the adverse symptoms from progressing during this period, doctors recommend the expectant mother more rest and limit physical exertion.
Any psycho-emotional stress is also excluded. Proper and rational mode of the day is a very important task.
Danger for the future mother and fetus
The shortening of the cervix can lead to a significant threat to the course of labor. This condition threatens the development of cervical insufficiency. This pathology can lead to premature labor.
Strong physical exertion in this case may contribute to the deterioration of the general condition of the mother and her baby. Without medical intervention in such a situation is not enough.
If the mucous membranes of this organ begin to soften strongly on the background of shortening, the lumen of the neck expands. This contributes to The risk of infection of the baby increases many times. This situation also contributes to the penetration of pathogenic microbes into the uterine cavity and into the cervical canal.
Too short uterus, according to statistics, leads to an increase in preterm labor.Doctors note that women suffering from this pathology may need to have an emergency birth at 34-37 weeks of pregnancy.
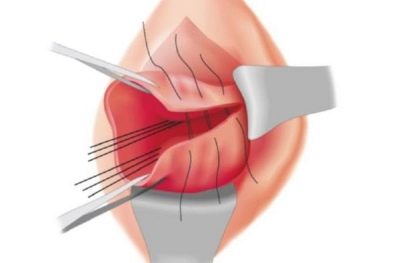
The narrow and short uterus, especially in miniature women, contributes to the fact that during childbirth they may have various injuries and tears. In this case, stitching may be required. Such a condition requires a longer rehabilitation and can significantly aggravate the first weeks of life after the long-awaited labor.
The risk of developing such a pathology is significantly increased in women who are carrying too large a baby or several children at the same time.
Quite often, a short cervix leads to the development of its hypertonus. This pathology also increases the risk of preterm labor. This condition is manifested by the appearance of pain in the abdomen, bleeding from the vagina, dizziness and severe fatigue. To identify this pathology can only obstetrician-gynecologist during the extended gynecological examination.
If the hypertonus on the background of the short cervix is detected already in late pregnancy, then in a dangerous situation, even hospitalization may be required. In this case, the expectant mother will be treated intensively in a hospital. “To be preserved” in this situation will also be offered to women with multiple pregnancies.
What to do?
It is important to note that if a woman has a short cervix before the pregnancy, the woman should regularly visit her gynecologist. This is necessary in order to monitor the status of this body. Quite often, shortening the uterus leads to the development of many dangerous pathologies.
However, in most cases, this pathological condition is determined only during pregnancy. Identifies his gynecologist during the examination of the future mother on the chair. If violations are detected, the doctor should refer the woman for additional transvaginal ultrasound examination.
Compliance with the mode of the day
Doctors recommend future mothers to strictly monitor what they do during the day. The daily routine is very important. In order to normalize the tone of the uterus, you should definitely get enough sleep. Sleep at the same time should be at least 8-9 hours a day.
To ensure that the cervix does not diminish further, expectant mother should monitor their excessive emotions. Strong anxiety or excitement over trifles leads to disruption of the nervous activity and spastic reduction of smooth muscles. Such a condition can only enhance the shortening of the cervix.
Optimal physical exertion helps the future mom to maintain the tone of the female muscles of the genitals. For its normalization, while practicing yoga for pregnant women or regular walks in the fresh air. Also, to prevent the deterioration of this pathology, doctors forbid the future mom to lift weights.
Normalization of overweight is a very important condition for maintaining the health of the female genital organs. During pregnancy, the expectant mother already gains weight. This is due to the growing baby in her tummy, as well as the entire mass of all placental membranes. Too much weight can lead to compression of the reproductive organs, which also provokes shortening of the cervix.
In some cases, doctors may recommend that women who suffer from this pathology wear special bandage. It helps to fix certain parts of the spine, and also somewhat reduces the likelihood of premature birth.
It is recommended to wear such bandages, as a rule, 4.5-5 months before delivery. The obstetrician-gynecologist after carrying out clinical examination writes out the wearing of these orthopedic means.
Shortening the cervix is not a contraindication for sexual intercourse.Only in certain acute pathologies can doctors recommend women to restrict sexual activity. As a rule, such recommendations are given to expectant mothers in the final stages of their pregnancy.
Gynecological treatment
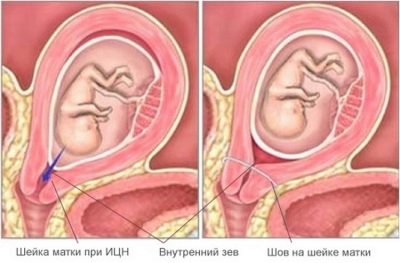
If, against the background of a short cervix, a woman develops cervical insufficiency, then she will need special methods of treatment. In this case, doctors usually put stitches that fix the shed of the uterus. They will be removed already just before birth.
Some of the methods are surgical and are performed under operating conditions. As a rule, in this case, a mandatory intervention of the anesthesiologist is required.
Cervical cerclage - This is an invasive procedure, which is carried out to correct disorders that have arisen on the cervix. In this case, temporary seams are superimposed on the cervix. They are necessary in order for it to remain “closed” until the birth itself. Usually, in this situation, the stitches are applied until 26-27 weeks of gestation, as this measure will be ineffective in the future.
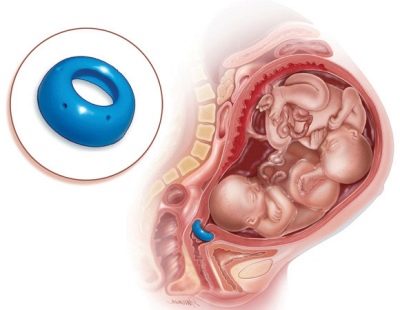
Another method of treatment of cervical insufficiency caused by too short cervix, is the imposition of obstetric pessary. This special device is inserted into the cervical canal and fixes its pharynx from the inside. The obstetric pessary is installed by an obstetrician-gynecologist.
This procedure is invasive, therefore requires mandatory training. It is better that it was conducted only by an experienced and qualified doctor. After installing the obstetric pessary, doctors limit physical exertion and recommend expectant mothers to rest more.
Drug therapy
In some situations, doctors may recommend a hormonal treatment to the expectant mother. This is possible in cases where a woman’s pathological changes occurred against the background of the existing dishormonal disorders. In this situation, doctors prescribe remedies that compensate for the lack of specific female hormones.
"Utrozhestan" - This is one of the drugs prescribed for the correction of violations. Gynecologists may prescribe this drug at various periods of pregnancy. For a period of up to 12 weeks, the reception of Utrozhestan contributes to the attachment of the fetus to the wall of the uterus, as well as the beginning of its intrauterine development.
Taking this drug also significantly reduces the risk of miscarriage. By late weeks of pregnancy, the increase in progesterone blood is somewhat reduced. Such a physiological response is necessary for the expulsion of the fetus from the womb. In this case, taking "Utrozhestan" can lead to a deterioration in the course of the final stage of pregnancy.
This drug may be administered in the form of capsules or various candles. In most cases, it is taken three times a day. Dosages are selected individually, taking into account the weight of the patient, the presence of concomitant diseases, as well as the nature of the course of pregnancy.
Expectant mothers should remember that Any hormonal drugs should be prescribed by a doctor. Independent use of such funds can lead to the development of quite dangerous states for the fetus and its own health.
Short cervix is not a contraindication for pregnancy planning. With such a physiological feature, a woman can become a mother even more than once. For the normal course of pregnancy, only timely monitoring of the condition of the baby while it is in the maternal tummy is required.
It is better to determine the shortening of the cervix before conceiving a baby. The only exception is if this pathology arose in a pregnant woman directly during pregnancy. Timely diagnosis of this condition reduces the significant risk of developing various diseases in both the pregnant woman and her baby.
The length of the cervix during pregnancy should be described by the gynecologist Lyudmila Shupenyuk in the next video.