What is screening during pregnancy and how is it done?
One of the most exciting moments for a woman during the childbearing period is screening for congenital abnormalities of the fetus. They are carried out for all pregnant women, but not every expectant mother is told and explained in detail what kind of research it is and what it is based on.
In this regard, screenings are overgrown with a mass of prejudices, some women even refuse to undergo procedures in order to “not waste their nerves”. We will describe what this diagnostics is in this article.
What it is
Screening is screening, screening, sorting. This is the meaning of this English word, and it fully reflects the essence of diagnostics. Prenatal screening is a set of studies that allow calculate the risks of genetic pathologies.
It is important to understand that no one can say on the basis of a screening that a woman bears a sick child, this screening results are not reported.
They only show how high the risk of birth for a given woman is at her age, anamnesis, the presence of bad habits, etc., of a child with genetic abnormalities.
Prenatal screening during pregnancy was introduced at the national level and It became mandatory more than two decades ago. During this time, it was possible to significantly reduce the number of children born with gross developmental defects, and the prenatal diagnosis played a significant role in this.
The terms in which these studies are carried out, give the woman the opportunity to terminate the pregnancy, if an unfavorable prognosis is confirmed, or leave and give birth to a child with pathology, but do it quite consciously.
Fearing screening or refusing to pass it is not very reasonable. After all, the results of this simple and painless study do not oblige to anything.
If they are within the normal range, this only confirms that the child is doing well, and the mother can be calm.
If a woman is at risk, according to the test results, this does not mean that her baby is sick, but it may be grounds for additional research, which in turn can show the presence or absence of congenital abnormalities with a 100% probability.
Screening is carried out free of charge, at any antenatal clinic, at certain times of pregnancy. Recently, when pregnancy after 30 or 35 years is not at all considered to be an extraordinary phenomenon, such a study is of particular importance, because with age, and this is not a secret, the age risks of giving birth to a baby with anomalies increase.
What risks are calculated?
Of course, to provide all possible pathologies that a child may have, no medical technique is able to. Prenatal screenings are no exception.Studies only calculate the likelihood of a child having one of the following pathologies.
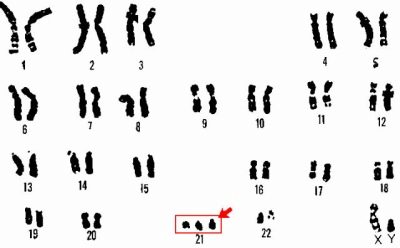
Down syndrome
This is a congenital change in the number of chromosomes, in which 47 chromosomes are present in the karyotype instead of 46. The extra chromosome is observed in 21 pairs.
The syndrome has a number of characteristics that a child is endowed with - a flattened face, shortening of the skull, a flat nape, shorter limbs, and a wide and short neck.
In 40% of cases, such children are born with congenital heart defects, in 30% - with strabismus. Such children are called "sunny" for the fact that they are never aggressive, they are kind and very affectionate.
Pathology is not so rare as it is thought.
Before the introduction of screening, she met in one of 700 newborns. After screening became ubiquitous, and women were given the opportunity to decide whether to leave a child with this syndrome, the number of “sunny” babies declined — now there are more than 1,200 healthy children per newborn.
Genetics have proved a direct relationship between the mother's age and the likelihood of Down syndrome in a child:
- a girl at 23 years old can get such a baby with a probability of 1: 1563;
- a woman at 28-29 years old has a 1: 1000 chance of having a “solar” child;
- if mother is more than 35 years old, but not yet 39 years old, then the risk is already 1: 214;
- a pregnant woman at the age of 45, such a risk, alas, is 1: 19. That is, out of 19 women at this age, one gives birth to a child with Down syndrome.
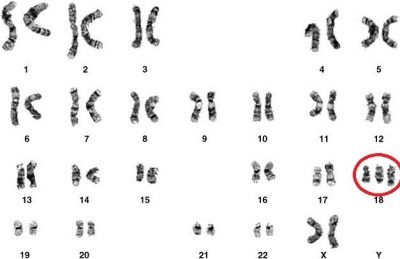
Edwards syndrome
Severe congenital malformation associated with trisomy 18 chromosome is less common than Down syndrome. On average, one in 3,000 children could theoretically be born with such an anomaly.
In the case of late-levers (after 45 years), this risk is approximately 0.6-0.7%. Most often, the pathology occurs in female fetuses. The risks of having such a baby are higher in women with diabetes.
Such children are born in time, but with low weight (about 2 kg). Usually in babies with this syndrome, the skull and the structure of the face are changed. They have a very small lower jaw, a small mouth, narrow small eyes, deformed ears — there may be no earlobe and a trestle.
The auditory meatus is also not always there, but even if there is one, it is severely narrowed. Almost all children have an anomaly of the structure of the foot of the "rocking" type, more than 60% have congenital heart defects. All children have anomalies of the cerebellum, severe mental retardation, a tendency to seizures.
Such babies do not live long - more than half do not live up to 3 months. Only 5-6% of children can live to a year, rare units that survive even after a year suffer from severe unreducible oligophrenia.
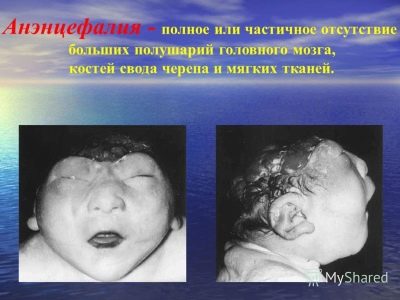
Anencephaly
These are neural tube defects that can occur under the influence of adverse factors in the very early stages of pregnancy (between 3 and 4 weeks). As a result, the fetus may be underdeveloped or in general there may be no cerebral hemispheres, there may be no vaults of the skull.
Mortality from such a defect is 100%., half of the children die in utero, the second half can be born, but only six of a dozen of them manage to live at least a couple of hours. And only a few manage to live for about a week.
This pathology is more common in multiple pregnancies, when one of the twins develops at the expense of another. The most frequently affected anomalies are girls.
Defect occurs on average in one case per 10 thousand births.
Cornelia de Lange syndrome
This ailment is considered hereditary, occurs in one case per 10 thousand births. It is manifested by severe mental retardation and numerous malformations.
Such children have a shortened skull, facial features are distorted, the ears are deformed, there are problems with eyesight and hearing, the limbs are short, and often there are not enough fingers.
Kids in most cases also have malformations of internal organs - the heart, kidneys, and genitals.In 80% of cases, children are imbeciles, they are not even capable of simple mental activity, they often cripple themselves, because do not control motor activity at all.
Smith-Lemli-Opitz syndrome
This disease is associated with a congenital lack of the enzyme 7-dehydrocholesterol reductase, which ensures the formation of cholesterol, which is necessary for all living cells in the body.
If the form is mild, the symptoms may be limited to slight mental and physical impairments, with severe form, complex defects and profound mental retardation are possible.
Most often, these children are born with microcephaly, autism, heart defects, lungs, kidneys, digestive organs, hearing, vision, severe immunodeficiency, curvature of the bones.
Each thirtieth adult on the planet is the carrier of this disease, but the “defective” DHCR7 gene is not always transmitted to offspring, only one out of 20 thousand babies can be born with this syndrome.
However, a frightening number of carriers forced doctors to include this syndrome in the definition of markers in prenatal screenings.
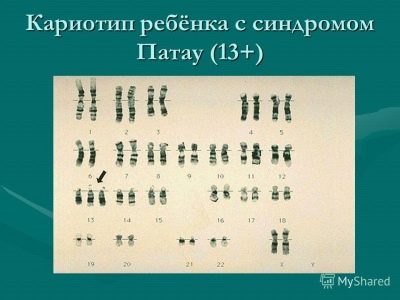
Patau syndrome
This is a genetic pathology associated with an extra 13th chromosome. Occurs on average once per 10 thousand deliveries. The likelihood of a baby with such a pathology is higher in “age-related” mothers. In half of all cases, such pregnancy is accompanied by polyhydramnios.
Children are born lightweight (from 2 to 2.5 kg), they have a decrease in brain size, multiple pathologies of the central nervous system, abnormal development of the eyes, ears, face, cleft, cyclopia (one eye in the middle of the forehead).
Almost all children have heart defects, several additional spleens, congenital hernia with a prolapse into the abdominal wall of most internal organs.
Nine out of ten babies with Patau syndrome die before they reach the age of one. About 2% of survivors can live to 5-7 years. They suffer from deep idiocy, are not aware of what is happening, they are not capable of elementary mental actions.
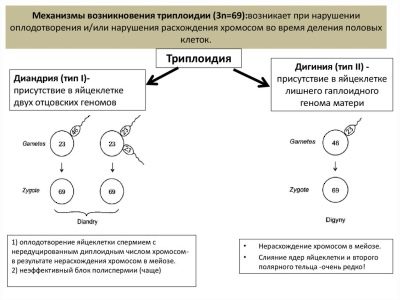
Non-molar triplody
An increase in the number of pairs of chromosomes at any level can be associated with an “error” at conception, if, for example, not one but two spermatozoids penetrated the egg cell, and each brought 23 pairs of chromosomes.
In combination with the maternal genetics in a child, not 46 chromosomes are laid, but 69 or another number. Such children usually die in utero. Newborns die within a few hours or days, since multiple defects, external and internal, are incompatible with life.
This is not a hereditary disease, it occurs by chance. And with the next pregnancy, the same parents have a minimal chance of repeating negative experiences. Prenatal screening also allows you to predict the possible risks of such pathology.
All the above pathologies, if their risk is high according to the results of screening and if they are confirmed as a result of an additional examination, which is appointed because a woman is in the risk group, are grounds for termination of the pregnancy for any medical reason.
There will be no forced abortion or artificial childbirth, the decision to interrupt remains with the pregnant.
Diagnostic methods
Prenatal screening methods are simple. They include:
- ultrasound, which, based on some characteristic markers, allows you to judge the possible presence of pathology;
- biochemical blood analysis from a vein, in which concentrations of certain substances and hormones are detected, certain values of which are characteristic of one or another congenital anomalies.
Three screenings are conducted during pregnancy:
For whom screening is required?
For all pregnant women who are registered, screening studies are planned and desirable. But no one can oblige a woman to donate blood from a vein and make an ultrasound scan as part of prenatal diagnosis - this is voluntary.
Therefore, every woman should think first of all the consequences of her refusal of such a simple and safe procedure.
First and foremost, screening is recommended for the following categories of pregnant women:
- expectant mothers who wanted to give birth to a child after 35 years of age (what a child it is in a row does not matter);
- pregnant women who already had children with congenital defects, including those with chromosomal abnormalities, had cases of fetal death due to genetic abnormalities in the baby;
- pregnant women who previously had two or more miscarriages in a row;
- women who took medicines, medicines that should not be consumed during pregnancy, in the early stages of fetal development (up to 13 weeks). These include hormones, antibiotics, certain psychostimulants, and other medications;
- women who conceive a baby as a result of incest (connections with a close blood relative - father, brother, son, etc.);
- future mothers who were exposed to radiation shortly before conception, as well as those whose sexual partners were exposed to such radiation;
- pregnant women who have relatives with genetic disorders in the family, as well as if such relatives are present on the part of the future father of the child;
- future mothers who are carrying a child whose fatherhood is not established, for example, conceived through IVF using donor sperm.
Description of the study - how is screening
It is impossible to call prenatal screening an accurate study, because it only reveals the probability of pathology, but not its presence. Therefore, a woman should know that the markers on which the laboratory technicians will rely and the computer program that calculates the probability can be detected in her blood. not only because of the pathologies in the child.
Thus, the concentration of certain hormones is increased or decreased as a result of the simplest common cold, ARVI, and food poisoning, which the pregnant woman suffered on the eve of the study.
Indicators may be affected lack of sleep, smoking, severe stress. If such facts take place, the woman must warn her doctor about this in consultation before she gets a referral for screening.
Each of the screenings is desirable to take one day, that is, the blood from a vein for biochemical research, and a visit to the ultrasound room should be done with a minimum time difference.
The results will be more accurate if the woman goes to the ultrasound immediately after donating blood for analysis. The results complement each other, the data of ultrasound and blood tests are not considered separately.
First screening and decoding of its results
This screening is also called 1-trimester screening. The optimal time for it is 11-13 weeks.
In a number of women's consultations, the terms may vary slightly. Thus, it is allowed to take the test at 10 full weeks, at week 11, and also at 13 full weeks before the obstetric period of 13 weeks and 6 days.
The screening begins with the fact that a woman is weighed, her growth is measured, and all the diagnostically important information that is needed to calculate the risks will be entered in a special form. The more such information is indicated, the higher the accuracy of the study.
The end result still produces a computer program, devoid of feelings and emotions, unbiased, and therefore the human factor is only important at the preparatory stage - the collection and processing of information.
Important for the diagnosis are: the age of parents, especially mothers, their weight, the presence of chronic diseases (diabetes, pathologies of the heart, kidney), hereditary diseases, the number of pregnancies, childbirth, miscarriages and abortions, bad habits (smoking, drinking alcohol or drugs), the presence of future mothers and fathers of relatives with hereditary diseases, genetic pathologies.
The first screening is considered the most important of the three. It gives the most complete picture of the health and development of the baby.
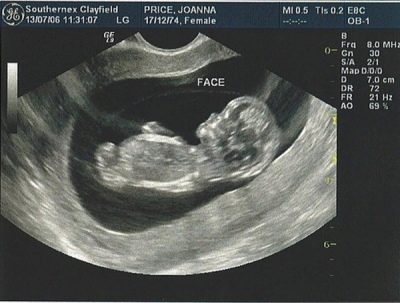
In the ultrasound diagnosis room, a woman is waiting for the most common ultrasound scan, which she probably already did to confirm the fact of a pregnancy.
On ultrasound in the screening study look:
- The physique of the crumbs - whether all the limbs in stock, whether they are located. If desired, the diagnostician can even count the fingers on the hands of the baby.
- The presence of internal organs - the heart, kidneys.
- OG - circumference of the head of the fetus. This is a diagnostically important indicator that allows you to judge the correct formation of brain lobes.
- KTP - the distance from the tailbone to the crown. Allows you to judge the growth rate of the child, as well as to clarify the duration of pregnancy with an accuracy of one day.
- LZR - the fronto-occipital size of the fetus.
- Heart rate - the heart rate of the baby, the diagnostician also notes whether the heartbeat is rhythmic.
- The size and location of the placenta, the place of attachment.
- The number and condition of umbilical cord vessels (some genetic pathologies may be manifested by a decrease in the number of vessels).
- TVP is the main marker that allows to judge the likelihood of the most common pathology - Down syndrome, as well as some other developmental abnormalities (Edwards syndrome, Turner syndrome, pathology of the structure of bones, hearts).
The thickness of the collar space is the distance from the skin to the muscles and ligaments at the back of the fetal neck.
Measured by TBP in millimeters, and thickening of this skin fold characteristic of children with chromosomal abnormalities and developmental defects is undesirable.
TVP rates for first trimester screening:
Gestational age | Collar space thickness |
10 weeks - 10 weeks + 6 days | 0.8-2.2 mm |
11 weeks - 11 weeks + 6 days | 0.8-2.4 mm |
12 weeks - 12 weeks + 6 days | 0.7-2.5 mm |
13 weeks - 13 weeks + 6 days | 0.7-2.7 mm |
Thus, if the child at week 12 TVP above normal values, and, not a few tenths of a millimeter, but much more, then an ultrasound is reappointed in a week or two.
A slight excess of the norm does not always speak about the pathology of the child. So, according to statistics, the diagnosis of "Down syndrome" in 12% of cases was confirmed with a TVP at week 13 of 3.3-3.5 mm, and for women who had a fetal TVP of 2.8 mm instead of the normal 2.5 mm, disappointing diagnosis was confirmed only in 3% of cases.
Excess rates by 8 mm from the upper limit and more - an indirect indication of the likelihood of Turner syndrome, an increase of 2.5 - 3 mm may be a sign indicating the likelihood of the presence of such pathologies as Down syndrome, Edwards syndrome, and Patau syndrome. After 14 weeks, the TVP is not measured, it has no diagnostic value. To complete the picture must laboratory data.
In addition to the TVP, the diagnostician will necessarily be regarded as an informative indicator of CTE (coccyx parietal size).
Norms KTR at the first screening:
Gestational age | Kopchik-parietal size (KTR) |
10 weeks | 33-41 mm |
11 weeks | 42-50 mm |
12 weeks | 51-59 mm |
13 weeks | 62-73 mm |
A very important marker of first trimester ultrasound screening is considered definition of the nasal bone in the fetus. Its absence (flattening) is characteristic of many congenital genetic pathologies.
The biggest experiences of future mothers are connected with this very bone, because not every pregnant woman has the opportunity to examine and measure it.If the baby is face inward, back to the ultrasound sensor, you will have to try to get the baby to roll over, if this does not bring results, the doctor will put a dash or write that it was not possible to measure the nasal bones.
Normally, the rules regarding this marker are rather arbitrary, because there are people with large noses, and there are people with small snub-nosed "buttons." This innate "nasal" theoretically can already be seen on ultrasound during the first screening. And a small nose may well be a hereditary feature, and not a sign of malformations.
Therefore, it is good if at the first examination the nose is already located, it is visible to the doctor.
If not, then you should not get upset, you can repeat the ultrasound scan in a couple of weeks or visit another specialist, because different people can see something or not see it in different ways, not to mention that ultrasound in different clinics is done on different devices. level
Nasal bone size (normal):
Gestational age | Length of nasal bone |
10 weeks | Most often it is not measured, not measured. |
11 weeks | Not measured |
12 to 13 weeks | 2.0-4.2 mm |
13-14 weeks | 2.9-4.7 mm |
The blood test in the framework of the first trimester screening is called the double test, since it determines the concentration two extremely important substances:
- PAPP-A - plasma protein, which determines only in pregnant women;
- HCG, more specifically β-hCG - human chorionic gonadotropin, the so-called pregnancy hormone.
Rates of hCG for a period of 10 to 14 weeks range from 0.5 to 2.0 MoM.
An increase in blood β-hCG may be an indirect sign of Down syndrome in a child, and a significant decrease in the level of this hormone may be a sign of Edwards syndrome.
Elevated levels of hCG may turn out to be quite healthy for children with multiple births, pregnant women with excess weight, with diabetes mellitus in history, as well as with gestosis during pregnancy, accompanied by edema, increased blood pressure.
Lowered HCG may also be due to the threat of miscarriageif it is present in this woman, as well as in case of delayed development of the baby, which may be accompanied by placental insufficiency.
Norms of plasma protein - protein PAPP-A:
- at the 11th week of pregnancy - 0.46-3.73 MDU / ml;
- at week 12 - 0.79-4.76 honey / ml;
- at week 13 - 1.03-6.01 honey / ml;
- in the 14th week of pregnancy - 1.47-8.54 IU / ml.
Since different laboratories use different reagents, methods of work, then the readings in two different laboratories, if a woman gives blood in both on the same day, may differ from each other. Therefore, it is customary, as in the case of hCG, to determine the concentration of a substance in MoM.
The norm of PAPP-A for the first trimester is an indicator that is in the range of 0.5-2.0 MoM.
Lowering PAPP-A is regarded as a risk marker for Edwards syndrome and Down syndrome, Patau. Also, a decrease in protein can talk about the death of the baby in utero, about his malnutrition with inadequate placental nutrition.
Raising the level of PAPP-A should not cause concern if all other markers detected as a result of screening (TVP, hCG are within the normal range).
If the doctor claims that the expectant mother has an elevated PAPP-A level, this may indicate that the placenta of such a woman can be low, that she has not one, but two or three babies, and that her baby is very plump, its parameters exceed the age. Sometimes an increase in the level of this plasma protein indicates an increased thickness of the placenta.
A woman will usually find out the results of screening in a few days or weeks. It all depends on how the accredited laboratory in the region works, how long the queue is.
To simplify the understanding of what is happening, obstetrician-gynecologists try not to load the expectant mother with numbers, lobes and MOM, they simply say that everything is in order or that additional research needs to be done.
The finished form of the first prenatal screening looks like a graph with explanations, just below - a computer program that summarized all the data about the woman and her health, the results of ultrasound and the concentration of hCG and PAPP-A, gives risks.
For example, Down syndrome - 1: 1546. This means that the risk is low, most likely, everything is fine with a child. If the risk is indicated as 1:15 or 1:30, then the probability of having a sick baby is high, more detailed diagnostics are needed to establish the truth.
Second screening and decoding of its results
The second screening is called screening for 2 trimesters. It takes place between 16 and 20 weeks. The most informative period is considered 16-18 weeks.
The study includes ultrasound diagnosis of the fetus, as well as biochemical blood tests - double, triple or quadruple test. When conducting a study it does not play a big role anymore, whether a woman will undergo both examinations at the same time.
Not so long ago, it was believed that if the first screen showed no abnormalities, then the second was not necessary at all, except for women at risk.
Now second trimester screening is considered equally voluntary as the first, however, its data do not already represent such an important diagnostic value as the indicators of the first study in the first trimester.
So, in the ultrasound diagnosis room, a pregnant woman is waiting for the usual and already familiar procedure, which will be carried out either transvaginally (if the woman is full and the view through the abdominal wall is difficult), or transabdominal (using a stomach sensor).
The diagnostician will carefully study the baby, assess its motor activity, the presence and development of all organs.
Specific markers, such as the thickness of the collar space, with ultrasound in the first trimester, in the second study there.
The overall development of the child is evaluated, and the data obtained are correlated with the variants of the average normative values for this age of gestation.
Fetometric standards for ultrasound screening for the 2nd trimester screening:
Obstetric term | BPR (biparient head size) mm | LZR (frontal-occipital size) mm | DBK (thigh length) mm | WPC (humerus length) mm | DKP (length of the bones of the forearm) mm | Og (Head circumference) mm | Coolant (abdominal circumference) mm |
16 week | From 26 to 37 | 32 to 49 | From 13 to 23 | From 13 to 23 | 12 to 18 | 112-136 | 88-116 |
17 week | 29 to 43 | 37 to 58 | 16 to 28 | 16 to 27 | 15 to 21 | 121-149 | 93-131 |
18 week | 32 to 47 | 43 to 64 | From 18 to 32 | From 19 to 31 | From 17 to 23 | 131-162 | 104-144 |
19 week | From 36 to 53 | From 48 to 70 | 21 to 35 | 21 to 34 | From 20 to 26 | 142-173 | 114-154 |
20 week | From 38 to 56 | 53 to 75 | 23 to 37 | 24 to 36 | 22 to 29 | 154-186 | 124-164 |
Deviations from the averaged parameters can speak not only of some pathologies, but also of hereditary features of appearance. Therefore, an experienced diagnostician will never frighten a pregnant woman by saying that her child has a too big head, if he sees that her mother’s head is also rather big, and her dad (who, by the way, you can take with you to the ultrasound room) also does not belong to people with a small skull.
Children grow up “jumps”, and a small lag from the norms does not mean that such a baby loses nutrition, suffers from hypotrophy or congenital diseases. Deviation from the standard values indicated in the table will be assessed individually by the doctor. If necessary, additional diagnostic procedures will be given to the woman.
In addition to the fetometric parameters of the baby, in the ultrasound diagnosis room at the screening of mid-pregnancy, a woman will be told about how the tot is located in space - up or down, and examine its internal organs, that it is very important to understand if there are any defects in their development:
- lateral ventricles of the brain - normally do not exceed 10-11.5 mm;
- the lungs, also, like the spine, kidneys, stomach, bladder, are indicated as “normal” or “N” if there is nothing unusual in them;
- The heart must have 4 cameras.
The diagnostician pays attention to the location of the placenta. If in the first trimester it was located low, then the chances that by the second screening the baby seat would rise are great. It is taken into account on which wall of the uterus it is fixed - on the front or back.
It is important that the doctor is able to decide on the method of delivery.
Sometimes the location of the placenta on the anterior uterine wall increases the likelihood of detachment; in this situation, cesarean section may be recommended. The maturity of the placenta itself in the period in which the second study is conducted has a zero degree, and the structure of the pediatric place must be uniform.
Such a thing kaIAG - index of amniotic fluid, indicates the amount of water. We already know that some congenital malformations are accompanied by low-flow water, but this index itself cannot be a symptom of genetic diseases. Rather, it is needed to determine the tactics of further management of pregnancy.
The norms of the amniotic fluid index:
Gestational age | Amniotic Index (mm) |
16 weeks | 71-201 |
17 weeks | 77-211 |
18 weeks | 80-220 |
19 weeks | 83-225 |
20 weeks | 86-230 |
Special attention in the study under the second screening is given to the state and features of the umbilical cord - the cord, connecting the child with the placenta. Normally, it contains 3 vessels - two arteries and one vein. On them there is an exchange between the child and mother. The baby receives nutrients and oxygen-rich blood, and metabolic products and blood containing carbon dioxide return to the mother.
If there are only 2 vessels in the umbilical cord, this may indirectly indicate Down syndrome and some other chromosomal abnormalities, but it is possible that the work of the missing vessel is compensated by the existing one and the child is healthy. Such babies are born weaker, underweight, but they have no genetic abnormalities.
The doctor will advise the pregnant woman not to worry about the missing vessels in the umbilical cord if other ultrasound indicators are within the normal range, and the double or triple test (biochemical blood test) does not show pronounced deviations.
A blood test is most often a triple test. The concentration of free hCG, free estriol and AFP (alpha-fetoprotein) is determined in the sample of the venous blood of the future mummy. These substances give an idea about the course of childbearing and the possible risks of genetic pathologies in crumbs.
The norms at different laboratories are individual, to summarize the various data used values in MoM. Each of the three markers ideally lies somewhere between 0.5-2.0 MoM.
Level of hCG in the second screening:
Obstetric term | Norm hCG (measured in ng / ml) |
16 weeks | 4,66-50,0 |
17 weeks | 3,33-42,7 |
18 weeks | 3,84-33,2 |
19 weeks | 6,75 |
20 weeks | 5,26 |
Increasing the level of this hormone in the second screening more often indicates that the woman has preeclampsia, she has edema, protein in the urine, she has taken or is taking certain hormonal drugs, for example, to save pregnancy.
Increased levels of hCG in women who have twins or triplets. Sometimes the increase in the value of this substance indicates that the term was set up erroneously, and an adjustment is required.
On chromosomal pathology such as Down syndrome can signal a significant excess of the upper threshold of hCG with a simultaneous significant decrease in the other two components of the triple test. Alpha-fetoprotein and the hormone estriol are pathologically underestimated.
The level of free estriol in the second screen:
Obstetric term | Estriol Norm (measured in ng / ml) |
16-17 weeks | 1,17-5,52 |
18-19 weeks | 2,43-11,21 |
20 weeks | 3,8-10,0 |
A slight excess of the concentration of this female hormone may be due to multiple pregnancies or to the fact that the woman bears a large fetus.
A decrease in this hormone may indicate a likelihood of neural tube defects, and Down syndrome or Turner’s disease, as well as Patau or Cornelia de Lange syndrome.Not every decrease in this substance is considered pathological; doctors begin to sound anxiety when the level is lowered by more than 40% of the average value.
A reduced level of estriol can sometimes indicate a heated Rhesus conflict, the threat of premature birth, and also insufficient placental nutrition of the child.
AFP level in the second trimester
Obstetric term | Norms AFP (IU / ml) |
16 weeks | 34,4 |
17 weeks | 39,0 |
18 weeks | 44,2 |
19 weeks | 50,2 |
20 weeks | 57,0 |
A significant excess of alpha-fetoprotein may be an indirect sign of the absence in the child of the brain, in whole or in part, of the pathological softness of the spine and other conditions inherent in congenital malformations of the neural tube.
For pregnant women, expecting twins or triplets, an increase in ACE is the absolute norm.
Reducing the level of this substance in the blood of the expectant mother can be an indication of a completely normal pregnancy, while in combination with elevated hCG and reduced estriol, this indicator sometimes indicates a possible Down syndrome.
If the fetus is completely healthy, a decrease in AFP sometimes accompanies maternal obesity or diabetes mellitus in a woman’s history. Low location of the placenta also affects the level of this substance, AFP may be below normal.
The results and results of the second trimester screening are also calculated using a special computer program, but already taking into account the data and the first screening study.
Only a doctor can help decipher the probability of the birth of a sick baby to a woman.
An experienced obstetrician-gynecologist is always personally "recheck" the prediction of the computercomparing the concentrations of individual substances with the history of the pregnant woman, her history, personal characteristics, as well as with the protocols of the first and second ultrasound.
Third screening and its results
The final, third screening of hereditary diseases and other pathologies of the fetus is carried out in 30-36 weeks. Most often, doctors try to prescribe a study for 32-34 week. The examination includes ultrasound, as well as a kind of result of two previous studies.
As part of the screening conduct CTG (cardiotocography), This method allows you to establish how the frequency of the heart of the toddler changes during its movements, how much the number of these movements is large.
Women at risk are not only carrying out an ultrasound scan, but also are assigned an USDG (Doppler ultrasound), which allows to evaluate the blood flow velocity in the uterine arteries. This allows you to make a more accurate picture of how the unborn baby feels, if he has a hypoxic state, or if he has enough nutrients.
On the ultrasound, the diagnostician reports the fetometric data of the child, its position in the uterus, the amount of water, and also assesses the thickness and degree of maturity of the placenta.
From 30 weeks the placenta is usually “aged” to 1 degree, and from 35 weeks to the second. According to the thickness of the children's place, the experts judge the ability of this temporary organ to satisfy the needs of the crumbs for nutrients.
The thickness of the placenta when held in third trimester
Obstetric term | Placenta Thickness (mm) |
30 weeks | 23,9-39,5 |
31 weeks | 24,6-40,6 |
32 weeks | 25,3-41,6 |
33 weeks | 26,0-42,7 |
34 weeks | 26,7-43,8 |
35 weeks | 27,5-44,8 |
36 weeks | 28,0-46,0 |
Become more thin than it is provided by the norms, the placenta can in thin and thin women, as well as in future mothers who have had infectious diseases during gestation.
The thickening of the children's place often indicates the presence of Rh-conflict, it is characteristic in the third trimester for women suffering from diabetes, preeclampsia. Placental thickness is not a marker of chromosomal abnormalities.
The fetometry of children in these terms may already differ significantly from the normative values, because everyone is born with different parameters, weights, each similar to their mom and dad.
Blood tests for biochemical markers in the third trimester do not pass.Limited to the usual list of tests - general blood and urine tests.
If screening showed abnormalities
If the verdict of a computer program analyzing the data obtained as a result of screening shows a high risk of having a child with developmental pathologies, chromosomal and hereditary diseases, this is unpleasant, but not fatal.
All is not lost, and the child may well be healthy. In order to clarify this issue in detail, invasive studies can be assigned to a woman.
The accuracy of such methods is close to 99.9%. They are told in detail to the expectant mother and they definitely give time to think about whether she really wants to know the truth at any cost, because somehow the procedures themselves, which allow an accurate diagnosis to be made, are a danger to save the pregnancy.
For a start, a woman is sent for consultation to genetics. This specialist "rechecks" the results issued by the computer, and also directs to invasive diagnostics.
For the study, not samples of the mother’s blood and tissues are taken, but tissue samples and the baby’s blood, as well as the amniotic fluid.
Any, even the safest, existing method - amniocentesis - is associated with the risk of losing a pregnancy. On average, the risk of infection and termination of pregnancy range from 1.5 to 5%. This can not be ignored by consenting to such a procedure.
If the results of the first screening were negative, a woman may be given:
- chorionic villus biopsy (for up to 12 weeks);
- amniocentesis (amniotic fluid sampling for analysis).
If the future mother and her treating doctor were alerted by the results of the second screening, It may be decided to conduct the following diagnostic procedures:
- amniocentesis;
- amnioscopy (visual examination of the ovum with the help of a thin flexible endoscope - performed only from 17 weeks of gestation);
- placentocentesis (sampling for the analysis of cells of the “children's place”, held from 18 to 22 weeks);
- cordocentesis (a child’s blood is taken for laboratory tests, it is carried out from week 18);
- fetoscopy (examination of the child with an endoscope and taking a piece of fetal skin for analysis. The procedure can be carried out from 18 to 24 weeks).
A thin surgical instrument can be inserted in three ways - through the abdominal wall, through the cervical canal and through a puncture in the vaginal fornix. The choice of a specific method is the task of specialists who know exactly how and where exactly a particular woman has a placenta.
The whole procedure is carried out under the supervision of an experienced, qualified ultrasound diagnostics doctor; everything that happens in real-time mode helps to track the ultrasound scanner.
The danger of such research is the possibility of early discharge of water, abortion. A crumb in the womb can get wounded with a sharp thin instrument, placental abruption, inflammation of the fetal membranes can begin. Mom can get wounded, the integrity of her intestines and bladder are at risk.
Knowing this, every woman has the right to decide for herself whether to agree to an invasive diagnosis or not. Make her go to the procedure no one can.
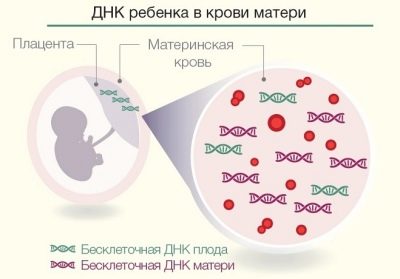
Since 2012, a new way of research has been conducted in Russia - non-invasive prenatal DNA test. Unlike the invasive methods described above, it can be carried out already at the 9th week of pregnancy.
The essence of the method is in isolating the DNA molecules of the child from the mother’s blood, since the baby’s own blood supply has been working for the baby since the 8th week of pregnancy, and some of its red blood cells enter the mother’s bloodstream.
The task of the technician is to find these red blood cells, extract DNA from them and determine whether the child has any congenital abnormalities. At the same time, the technique allows finding out not only the presence of gross chromosomal abnormalities, but also other gene mutations, which cannot be recognized by any other means.Also, mother with an accuracy of 99.9% will be told the floor of the baby as early as 9 weeks of pregnancy.
Such tests, unfortunately, are not yet included in the package of health insurance, and therefore are paid. Their average cost is from 40 to 55 thousand rubles. It is offered by many private medical genetic clinics.
The downside is that an invasive test with a puncture of the fetal bladder will still have to be passed if a non-invasive DNA test shows that there are deviations.
The results of such an innovative test have not yet been accepted by gynecological hospitals and maternity hospitals as grounds for termination of pregnancy for a long time for medical reasons.
Screening training
The result of screening in the antenatal clinic can be false both in a positive and in a negative direction, if a woman does not take into account the negative impact on her body of certain factors, such as medication or severe stress. Therefore, doctors recommend carefully preparing for the passage of a simple study.
Three days before screening It is not recommended to eat fatty, fried and spicy foods. This may distort the results of biochemical blood tests.
Diet also implies the rejection of chocolate, cakes, oranges, lemons and other citrus fruits, as well as smoked meats.
Donate blood should be on an empty stomach. But with a consultation you can take crackers or a small chocolate bar to eat it after giving blood before going through the ultrasound procedure.
A child under the influence of an eaten chocolate mom will move more actively, and will be able to "appear" to the diagnostician in all its glory. An empty stomach does not mean that for three days a woman should starve herself and her baby. To successfully donate blood to biochemistry, it’s enough not to eat at least 6 hours before taking blood.
For a week, all stress factors should be excluded, since the evening before the examination, a woman should take a drug that reduces the formation of gas in the intestine so that the “swollen” intestine does not cause compression of the abdominal organs and does not affect the results of the ultrasound examination. Safe for future mothers drug - «Espumizan».
It is not necessary to fill the bladder, at this time (10-13 weeks) the fetus is clearly visible without filling the bladder.
Research accuracy
The accuracy of second-trimester screening is lower than the similar characteristic of the first screening, although its results raise many questions. So, sometimes it turns out that a woman who was given high risks gives birth to a perfectly healthy baby, and a girl who was told that everything is “normal” becomes the mother of a child with severe genetic pathologies and developmental anomalies.
Exact research is considered only invasive diagnostic methods. The accuracy of screening detection of Down syndrome using blood tests and ultrasound by experts is estimated at about 85%. Trisomy 18 screening reveals with an accuracy of 77%. However, these are figures of official statistics, in practice everything is much more interesting.
The number of false-positive and false-negative screenings has recently increased. This is not due to the fact that doctors began to work worse. It’s just that many women who are hoping for the competence of paid specialists try to do research for their own money in a paid center, and there ultrasound examinations are not always carried out by specialists who have international access to conduct exactly this type of research.
The number of incorrect analyzes is also growing, since even living people work with modern equipment in laboratories.
There is always a chance that the doctor didn’t notice something on the ultrasound or didn’t see what was there, and that the laboratory assistants made an elementary technical error. Therefore, sometimes the data from one laboratory should be rechecked in another.
It is best to undergo a screening study in consultation at the place of residence - there doctors are guaranteed not only admissions to this kind of diagnosis, but also a lot of experience in carrying it out.
It is important to remain calm and believe that everything will be fine with the child, without giving up the opportunity to learn about the state of the baby as much as possible. Screening provides the opportunity.