Symptoms and treatment of pneumonia in infants
Inflammation of the lungs is among the ten most dangerous diseases that can lead to death. This disease is especially dangerous for infants, whose weak and “untrained” immunity is not yet able to cope with such an excessive load.
We will describe how to recognize and treat pneumonia in children under one year old in this article.
What it is
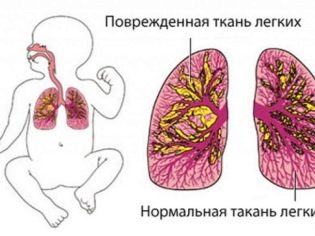
Pneumonia is a whole group of diseases united by a common symptom - inflammation of the lung tissue, alveoli. Most often, pneumonia is infectious. Lung tissue and alveoli may be affected only in some segments, and may be affected by whole lobes. With total pneumonia, the entire lung is affected.
Such inflammation may occur in isolation, but in children, the disease is more often secondary in nature, essentially acting as a complication of other diseases and conditions.
Pathological processes in the tissues of the lungs cause staphylococci, streptococci, Klebsiella, pneumococcus, hemophilus bacilli and other microorganisms, as well as some viruses and fungi.
Inflammation can proceed relatively easily, but in infants, the disease is usually moderately severe or severe., again due to weak immunity. Only one lung can become inflamed, and then it will be unilateral pneumonia, or both at once in cases of bilateral disease.
The older the child, the easier it carries the disease, the "critical" age is considered to be up to 5 years.
According to the observations of pediatricians, pneumonia in young children often occurs between the ages of 3 and 9 months.
With the spread of antibiotics, pneumonia has ceased to be considered a fatal disease, but babies up to one year old who have very weak immunity still die from pneumonia. Mortality in this age group is about 40%.
The reasons
In infants, pneumonia can be congenital or acquired. In the first case, the lungs of the baby suffer even in utero, in the second - after birth. The development of the disease contribute to the following conditions:
- prematurity;
- intrauterine hypoxia;
- birth trauma associated with hypoxia and suffocation;
- Congenital heart defect;
- congenital malformations of the lungs;
- malnutrition, low birth weight;
- cystic fibrosis;
- HIV infection.
The basis of the disease is always a delay of bronchial secretions. Toddlers not only have a weaker immunity than in adults, but they do not know how to expectorate sputum if it accumulates. The accumulation of sputum is a favorable breeding ground for pathogenic bacteria.
In congenital pneumonia, infection often occurs through the blood, by hematogenous means. Acquired disease - most often a consequence of the disease, in which the upper respiratory tract suffered, and the infection was able to "fall" down into the lungs.
Also, the disease can begin in a child who, during the first hours, days and months of life, had to connect the ventilator. In this case, talk about post-traumatic pneumonia.
There is also one more physiologically caused reason for the development of pneumonia in children. it anatomical features of the respiratory system in infants.
The mucous membranes in babies are very loose, they are better supplied with blood, the permeability of blood vessels is higher, which means that such membranes swell more quickly with the disease. The airways are narrow, and any swelling, or accumulation of bronchial mucus, can cause such a serious complication as pneumonia.
Symptoms and signs
Congenital forms of inflammation of the lung tissue become apparent to doctors almost immediately after the baby is born. In any case, in the next few hours, neonatologists will be able to get all the results of the tests, suggesting that the baby has pneumonia.
Symptoms of a congenital disease in the first days after birth are manifested as:
- the baby has signs of oxygen starvation;
- the tone of all muscles is reduced - the child sucks poorly and languidly, if at all, does it, his arms and legs hang limply;
- the skin has pronounced signs of cyanosis - the color varies from bluish to lilac;
- the temperature is unstable - it can rise up to 39.5 degrees in children born on time and lower to 34.0-35.0 degrees in premature babies;
- in most cases, there is no respiratory and swallowing reflex - the child needs mechanical ventilation and nutrition through a probe;
- increased drooling.
If the infection occurred at the time of delivery or after them, the symptoms may appear after a couple of days, or after a couple of weeks, when the unsuspecting mother will be at home with the baby.
The first signs of the development of the inflammatory process in the lung tissue are as follows:
- disturbance of appetite, refusal of breast or bottle with mixture;
- indigestion, bloating, increased flatulence, diarrhea, copious and frequent regurgitation;
- cyanosis of the nasolabial triangle, cyanosis of the tongue;
- pale skin;
- uneven breathing with “wheezing”;
- shallow cough.
Quite often in infants of the first year of life, the pneumonia has no pronounced symptoms at all, occurs in a latent form, without fever and cough, and this is the most dangerous scenario. Only attentive attitude to the child will help to suspect that something was wrong.
Hidden forms of illness are characterized by constant feeling of thirst, lethargy, drowsiness, problems with appetite, slow weight gain or weight loss.
Diagnostics
If any symptoms appear that may even indirectly indicate a possible pneumonia, parents should immediately contact a pediatrician.
The doctor will carefully examine the skin of the child, assess their color, listen to the lungs - a special noise “color” of the inhalation and exhalation is characteristic of pneumonia. After that can be assigned:
- X-rays of light;
- computed tomography of the chest;
- sputum collection for analysis (to determine the type and type of pathogen);
- general and detailed blood tests;
- blood test for gas (to determine the degree of oxygen starvation).
Most often, to conduct a thorough examination of the child has to be hospitalized, because in the hospital there is an opportunity to carry out all diagnostic procedures quickly, because the earlier the treatment is started, the more favorable the prognosis will be.
Treatment
Therapy for pneumonia begins with the use of antibiotics. The baby is prescribed intramuscularly or in the form of a suspension (with focal, localized pneumonia). Depending on the type and type of pathogen choose one or another antimicrobial drug.
First-line antibiotics in infants are considered penicillin group drugs. The most difficult thing is to choose a treatment for hospital pneumonia, since the microbe that a baby could get in the maternity hospital or hospital of a children's hospital is incredibly resistant to most existing antibiotics. It is during hospital pneumonia that a fatal outcome is most likely.
To facilitate the discharge of sputum, the child is prescribed special drugs - mucolytics in the form of syrup.Inhalations with them are useful for older children, it is difficult for the infant to perform the inhalation procedure.
With a severe course of the disease can be assigned hormonal drugs. For oxygen starvation, the child is prescribed an oxygen mask.
If a child enters the hospital with symptoms of intoxication (which is more than half of infants with pneumonia), then detoxification therapy is indicated - intravenous administration of saline with mineral, vitamin preparations.
To speed up the discharge of bronchial secretions, mother or another adult who is with the infant in the hospital are trained in the technique of vibratory massage based on vibrating finger tapping in the area of the bronchi and lungs.
Compliance with all recommendations and prescriptions, as well as properly selected medications can cure a child. 10-14 days.
Doctors sometimes allow to treat mild forms of pathology at home. Naturally, all traditional methods and methods for the treatment of pneumonia in infants are strictly contraindicated.
Prevention
The only convincing opportunity to protect infants from pneumonia is a pneumococcal vaccine. In 80% of cases, it is this pathogen that causes disease in young children. Vaccine against pneumococcal infection is administered free of charge. Since 2014, this vaccine has been included in the national preventive vaccination calendar.
American vaccine Prevenar is administered to children in 2 months.
A child who is not at risk has been born full-term, has no congenital heart defects, and can be recommended to be vaccinated from 3 months of age.
The vaccination schedule for pneumococcal infection looks like this:
- 2-3 months;
- 4.5 months;
- 6 months.
Revaccinate the child in one and a half years. The number of reactogenic vaccination does not apply, most babies perceive it without any side effects.
It is not to say that the vaccine completely eliminates the risk of infection, but even if pneumococcus enters the body of a vaccinated child, it is unlikely that it can cause pneumonia and other serious consequences, because the infection will flow easily. By the way, this vaccine is also will protect the baby in terms of the likelihood of developing severe bacterial otitis, meningitis, tonsillitis.
From 10 to 20% of children's pneumonia are associated with another pathogen - a hemophilic bacillus. There is also a vaccination from it, and it coincides in time with a vaccination against pneumococcal infection. It also rarely causes any negative effects on the child’s body.
The following recommendations can be attributed to non-specific measures of prevention of pneumonia:
- A child of the first year of life should be more carefully protected from possible infection with influenza, ARVI and other viral diseases, which may be a complication of pneumonia.
- If the baby is breastfed, lactation should be maintained, albeit until the child reaches 1 year of age. Mom's milk provides additional antibodies to various viruses and bacteria.
- The child should spend more time outdoors. And parents should air the baby room several times a day, do a wet cleaning in it, maintain the correct temperature and humidity.
- At a temperature of 20-21 degrees of heat and relative humidity of 50-70%, the risk that bronchial mucus, even in a child already sick, will thicken and cause an inflammatory process in the lung tissue, is minimal. The hotter the air in the room and the drier the air, the faster the mucus in the bronchi and nasopharynx turns into clots and crusts.
- All colds and other diseases associated with the manifestation of respiratory symptoms, occurring with cough, runny nose, should be treated in a timely manner, not letting them drift. Children under one year should definitely be shown to the doctor regularly.
- If the baby is still sick with SARS or flu, as well as any other diseases with respiratory manifestations, then the parents must ensure him peace and plenty of warm drinks. Enhanced drinking regime will help prevent thickening and drying of bronchial mucus.
- During pregnancy, the expectant mother must visit the antenatal clinic, in time to pass all the necessary tests, so that in the event of a staphylococcal or pneumococcal infection in time to receive the necessary treatment. This will reduce the risk of congenital pneumonia in the baby.
About what to do with pneumonia in children, see the following video.