Ultrasound in the 12th week of pregnancy: fetal size and other features
At the 12th week of pregnancy, the first routine ultrasound is most often performed. It will be accompanied by additional research, including laboratory. At this time, doctors and future parents can get a lot of interesting information about the state of health of the baby. How is the diagnosis at this stage of childbearing and what are the parameters of the crumbs, we will tell in this material.
Objectives of the survey
Ultrasound at the end of the third months of pregnancy is an integral part of screening aimed at identifying the likelihood of possible genetic pathologies. Together with the analysis of the blood of a pregnant woman, this method of research provides informative data, allowing to calculate individual risks of the birth of a child with malformations.
Screening prenatal study is usually scheduled for one of the days in the period from 11 to 13 week. 12 weeks is the most optimal time for diagnostics, since the information content of all indicators of interest to the doctor at this stage is as high as possible.
Ultrasound examination at this time allows:
- identify markers that indirectly indicate the likelihood of a child with Edwards, Turner, Down syndrome, Cornelia de Lange disease, Patau syndrome, neural tube abnormalities, which lead to brain development pathologies;
- check the period of pregnancy, determine the expected date of birth;
- find out the particular features pregnancy - multiple pregnancy she or usual, complicated or not;
- find out how the fetus feels, assess its vital activity, its size, compare it with the developmental norms inherent in this period;
- to identify problems with the reproductive health of the mother, if any, to eliminate the threat of miscarriage, detachment of the ovum and other pathological conditions.
Method and preparation
Often, an ultrasound scan at 12 weeks is called genetic ultrasound. The attitude towards him is appropriate. With anxiety and trepidation, future mothers are waiting for the day of the survey, because the word “screening” is scary and causes a lot of concern. Anxiety is superfluous, according to experts After all, this ultrasound has no peculiarities compared to similar diagnostics on other terms, no. Everything will be easy, familiar and painless.
The results of ultrasound at this time can be adversely affected by the accumulation of intestinal gases, which “push” the pelvic organs and squeeze them. Therefore, a couple of days before the screening study, you should not eat cabbage, legumes, carbonated water. A few hours before going to the doctor should take "Simethicone" or "Espumizan». These drugs will help eliminate intestinal gas residues and prepare for the examination.
Ultrasound at 12 weeks is done on the same day with laboratory blood sampling from a vein, which is necessary to establish the level of hormones and proteins responsible for the normal development of the baby and the correct flow of gestation. On the results of this analysis, which is conducted biochemical research method may affect food, bad habits of the mother, for example, smoking.
In order to get more reliable results, doctors do not recommend a woman to eat fatty foods, smoked and fried foods with a lot of spices, as well as sweets for 2-3 days before the examination.
On the day of the examination in the consultation should come on an empty stomach. Before undergoing this ultrasound, the woman weighs, measures growth, tells the attending physician all the data about previous diseases, her previous pregnancies and childbirth.
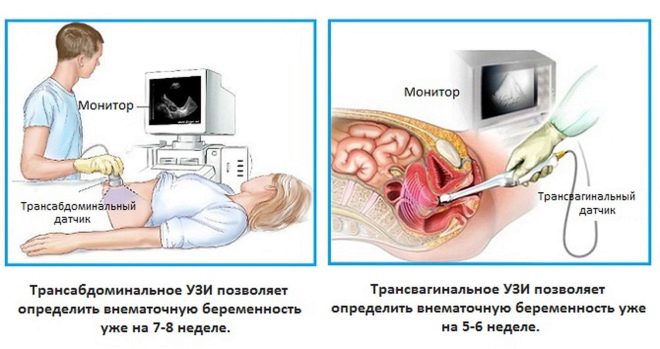
Ultrasound scanning at this time is carried out mainly by the transvaginal method, which is popularly called “internal ultrasound”. Filling the bladder is not required, the doctor gets access to the review through the vaginal wall, bypassing the bladder area. 12 weeks is considered a borderline period at which doctors can begin to use the transabdominal method for diagnosis - external ultrasound, when the sensor is only guided through the woman's abdomen, receiving a picture through the anterior abdominal wall.
The choice of method remains with the doctor, and much can affect him, including the constitution of the very future mother. If a woman is plump, there is a noticeable fatty “layer” on her stomach, then most likely the doctor will choose a vaginal method of examination. Thin patients have a greater chance of having an abdominal ultrasound scan during this period. In some cases, the doctor may use both methods.
What can you learn?
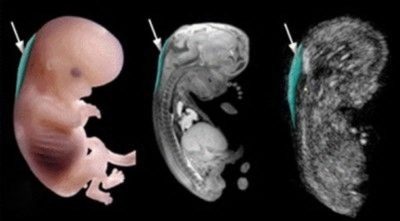
At this period, the baby becomes very similar to the little man, he has hands and feet. The tail, which was at the embryo, completely disappeared. Fingers separated on the arms and legs, the pads of the fingers this week acquire individual features - a unique pattern that is an imprint.
All the internal organs of the crumbs are fully formed, many of them (kidneys, liver, intestines, pituitary, heart) have already begun to function. The fruit itself weighs about 14-15 grams, its growth is on average from 45 to 80 mm. The kid is very active, he has already learned to use the handles, he can play with the umbilical cord or suck a finger. If the ultrasound diagnostician finds him at these sessions, he will definitely show the expectant mother what her grown-up baby is capable of.
The baby has already formed external genitals, and therefore with a favorable arrangement of the child, the doctor may already try to determine his sex. If the mother’s tummy lives twins or triplets, the doctor will be able to review and evaluate the parameters of each of the babies.
Not all of the above can be seen at week 12 using ultrasound, because not every consultation has a modern scanner with high resolution and detail.
But any device at this time will show how the fetus is moving, mom will be able to hear his heart beating, the size of the fetus can also be easily determined.
During the procedure, the doctor must examine probability of genetic pathologies according to their characteristic markers (visual signs). In addition, he will give an opinion on the health of the mother and tell you what to do if there is a threat of miscarriage, although at this time she, if she was, usually disappears, the state of the mother and the fetus returns to normal, and toxicosis begins to recede.
Decoding results
It is impossible to judge whether the child has the probability of genetic pathologies, many of which are lethal, and the rest simply do not leave a chance for healing the toddler by 12-week ultrasound alone. Therefore, doctors are deciphering the screening, comparing what the doctor saw on the scanner monitor and what the results of the biochemical examination of the blood of the pregnant woman showed.
Therefore, expect that after the ultrasound will know whether the baby is healthy, not worth it. We'll have to wait for the lab tests to be ready. After visiting the ultrasound room, a woman will be given a study protocol in which, using numbers and letter abbreviations, will “encrypt” basic information about the development of pregnancy.Let's look at what these cuts mean and what norms are characteristic of this week of gestation.
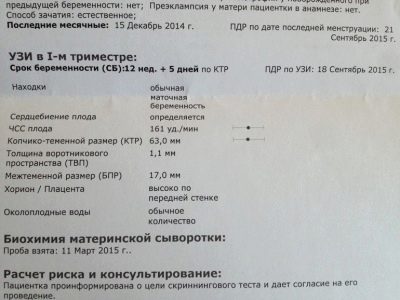
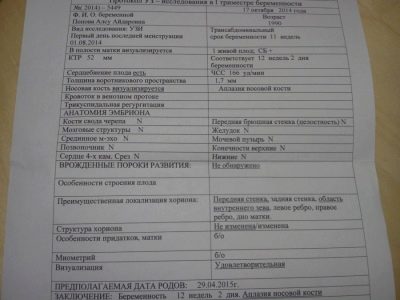
At the very beginning of the protocol, it describes how the study was conducted, and also indicated the date of the first day of the last menstruation - it is the basis for calculating the obstetric period and the date of birth. The following is a general picture of what the doctor saw. Indicate the number of fetuses in the uterus with the obligatory indication whether they are viable, whether they have signs heartbeat.
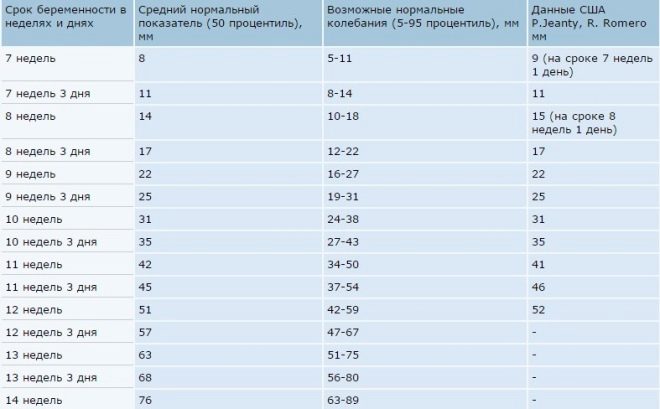
An important value that allows to judge the duration of pregnancy and the pace of development of the baby is the size from crown to tip of the coccyx, the so-called coccyx-parietal size, or CTE. This week, its average values are presented below.
Table of standards of KTR in the period of 11-12 weeks and 12-13 weeks:
| Term gestation (week + day) | Kopchiko-parietal size (KTR), mm - norm | KTP - fluctuations within normal limits, mm |
| 11+1 | 44,7 | 38,6 – 50,8 |
| 11+2 | 46,3 | 40,2 – 52,5 |
| 11+3 | 48,0 | 41,8 – 54,2 |
| 11+4 | 49,6 | 43,4 – 55,6 |
| 11+5 | 51,3 | 45,0 – 57,6 |
| 11+6 | 52,9 | 46,5 – 59,3 |
| 12 weeks exactly | 54,6 | 48,0 – 61,1 |
| 12+1 | 56,3 | 49,6 – 62,9 |
| 12+2 | 57,9 | 51,0 – 64,5 |
| 12+3 | 59,5 | 52,7 – 66,0 |
| 12+4 | 61,0 | 54,3 – 67,6 |
| 12+5 | 62,6 | 55,7 — 69,5 |
| 12+6 | 64,0 | 57,1 -71,0 |
The following is described. fetal heartbeat. The abbreviation of heart rate (heart rate) is complemented by a number. It indicates the speed with which the baby's heart beats. At this time, a normal value of 162 beats per minute is considered normal. The questions should not cause any value that ranges from 150 to 175 beats.
If the doctor does not like the frequency, he thinks that the heart of the baby beats slowly, unevenly, irregularly, too often, he will definitely report it. If this has not sounded, do not "wind up" yourself over trifles.
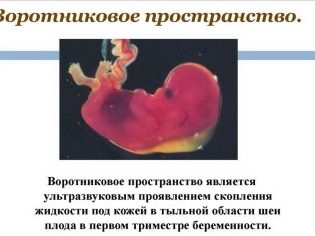
Next, the doctor proceeds to the main part, for which screening is being conducted - the study of markers of chromosomal pathologies. There are only two such signs on ultrasound in this period - the thickness of the collar space (TVP) and the nasal bones (well, if they are visualized, it is even better if they can be measured).
The space between the skin and the muscular skeleton on the back of the neck in children with various genetic diseases is noticeably thickened due to accumulation in this area of fluid. For example, babies with Down syndrome tend to shorten the neck.
The TVP as an indicator is informative only at this time, after 14 weeks it is not defined and can no longer tell anything. The nasal bones in children with a number of genetic pathologies flatten, and therefore they may be very small in a child with severe developmental abnormalities, or may be absent altogether. This marker may also indicate likely problems.
Collar thickness and length of the bones of the nose at 12 weeks:
Gestational age | TVP, mm | Nose bones, mm |
11-12 weeks | 1.6 (fluctuations from 0.8-2.4) | 2.3 (fluctuations from 1.8 to 2.9) |
12-13 weeks | 1.6 (fluctuations from 0.8-2.5) | 2.4 (fluctuations from 1.8 to 3.1) |
In a separate column rendered description of the anatomy of the embryo (fetus). There will not be any numbers, but only the signs “+” or “-”, which means that the body is either present or absent. The doctor may also indicate the "norm", "without features", "examined" or make data on the identified pathology.
To fill this part of the study protocol, the bones of the cranial vault, the main structures of the brain (“butterfly”), the spine, the 4-chamber heart section, the baby’s abdominal wall, the stomach, the bladder, the fetal stomach, the intestines are examined at 12 weeks. Separately, count the number of limbs, if there are two arms, and the legs are the same, then the doctor will indicate that they have been examined and are normal.
Determined by chorion position - A young placenta, which barely had time to form. It is determined on which wall of the uterus the “baby seat” is fixed. This is usually the back wall, but the presence of the chorion on the front wall should not frighten at all. The distance from the internal pharynx to the chorion is measured, and on the basis of this indicator, it is established whether the placentation is sufficient, low, or present.
Must be measured thickness of the placenta. Its abnormal growth can also indicate either infection of the fetus, or genetic abnormalities. Normal indicators for this period - from 14.5 to 15.5 mm.
Diagnostic Ultrasound examines the condition of the uterus, appendages, ovaries, measures the length of the cervix and indicates whether everything is normal, whether there is a risk of abortion.
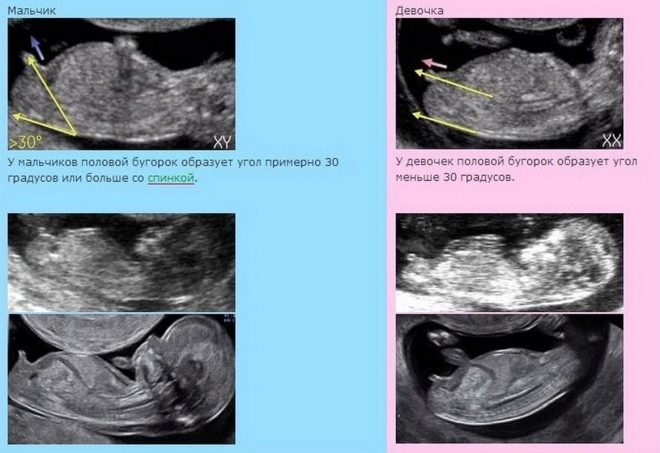
Gender definition is not included in the required screening parameters. If a woman wants to ask this question to the doctor, you will have to pay at the rate of female consultation for the provision of paid services (within 500 rubles). However, no doctor will be able to guarantee the accuracy of determining the sex in this period. There is too much risk of mixing up the genitals with the umbilical cord or the limbs, not to see or distinguish the boy from the girl, as they are still very similar.
Experienced doctors manage to see gender. The accuracy of the “prediction” in the first trimester is from 75 to 80%. More precisely, you can see the floor on the next scheduled ultrasound study at 18-20 weeks.
Possible problems
As part of an ultrasound scan at 12 weeks, some inconsistencies and problems can be identified. The most common situations are:
KTR is less than normal. The reasons for this deviation may lie in a later ovulation, that is, the fetus is younger than the doctor thinks and the pregnant woman herself. In this case, another ultrasound is prescribed, after 1.5-2 weeks. Significant deviation of this value from existing averaged standards may indicate development problems, which may be the result of bad habits, malnutrition of a pregnant woman, as well as insufficiency of the hormone progesterone in her body. When the coccyx-parietal size decreases, congenital pathologies of a genetic nature are not excluded. In this situation, additional research is needed.
- No nasal bones or they are less than normal. The absence of nasal bones (aplasia) or their small size increases the risk of developing a baby with chromosomal abnormalities, however, the accuracy of ultrasound as a diagnostic method does not always allow us to judge the presence of pathology. The doctor may not see the nose due to outdated equipment with low resolution. In addition, a small nose can be a hereditary individual trait, if one of the parents has a small nose, a “button”.
To understand the reason, the results of biochemical blood tests will help, as well as control ultrasound in a few weeks.
- TVP more than normal. A slight excess of this value should not cause alarm. For specialists, it is considered “critical” to exceed the size of the neck area 6–8 mm above the upper limit. In this case, the woman is sent for consultation to the genetics, additional invasive methods are prescribed - a chorionic biopsy or amniocentesis, in order to identify the pathology with an accuracy of 99.9% or to refute the suspicions. A significant excess of the parameter should be supported by changes in blood formulas, in particular, high levels of hCG and reduced levels of PAPP-A protein.
- Low placentation, previa. Of course, these conditions are quite dangerous in terms of the possibility of losing a pregnancy, but the forecasts are mostly positive, because the uterus grows every day, and the placenta rises along with stretching of the uterus walls (chorion at 12 weeks). The woman is prescribed a sparing mode of labor, bedridden mode can be displayed with the previa. Women are prescribed medications that have a positive effect on vascular permeability (“Actovegin"," Curantil "), as well as vitamin complexes designed specifically for expectant mothers.
- The threat of interruption, retrochorial hematoma. With such problems of gestation, the results of the ultrasound at this time only confirm the disturbing symptoms that a woman is experiencing - it may be bloody or serous discharge, as well as pain in the lower abdomen and in the lumbar region.In this case, the decision on treatment is made by an obstetrician-gynecologist, who either directs the woman to the hospital to preserve the pregnancy, or makes recommendations for treatment at home, if the hematoma (abdominal detachment) is not extensive.
In general, the forecasts are quite positive, and with all the doctor's appointments and respect for themselves, 95% of women manage to keep the pregnancy and give birth to a healthy and beautiful baby in time.
Research accuracy
In the final part of the protocol for screening ultrasound, a woman can read that the results of the study do not guarantee the birth of a healthy child. The question arises - why then pass the screening, if there is no clarity? The fact is that ultrasound is not considered to be an absolutely accurate method, the error and the error correction are between 10 and 15%. Thus, the accuracy of ultrasound on this period is equal to about 90%. When determining the baby's gender at 12 weeks, the accuracy is lower - 75-80%.
Ultrasound diagnosis at this time does not aim to establish specific diagnoses for the mother or baby. Diagnosis only contributes to the overall risk assessment of the appearance of a sick toddler in this woman, and also allows you to monitor the pace of development of a tiny person. Separately from the results of blood biochemistry, the conclusion of an ultrasound scan is not considered and cannot speak about the presence of a sick baby in a woman.
Common Questions
Both before the examination procedure and after it a lot of pregnant women have a lot of questions. Answers to the most common ones are presented below:
Sex by heart rate. Popular rumor ascribes to male fetuses a rarer heartbeat than girls. It is believed that in future little princesses the heart knocks often, “fearfully”, whereas in boys the rhythm of the heartbeat is measured, precise. From the point of view of medicine, it is impossible to assert that different sexes are characterized by a different heart rate. By gender, this indicator is not divided. However, experienced midwives in the distant past, when an ultrasound scan was not available, that was the way the sex of the unborn child was determined, however, they were mistaken in about 50% of cases.
There are some differences in the tone and rhythm of the heartbeat, but in the very late stages of pregnancy. At 12 weeks, it’s not worth judging the field of a child by the speed of a small heart.
- 3D ultrasound. The three-dimensional image, more familiar to the patient's unprofessional gaze, attracts and attracts every future mother. I'd like to look at my baby "in all its glory." But 12 weeks is too short a time to conduct such a study. The best for 3D ultrasound are the terms from 20 weeks and more. But also on an ordinary ultrasound scan, which takes place in the first trimester, you can ask for a baby’s picture that already looks not like a pea pod or an odd spot, but quite humanly.
- Ultrasound pictures. These pictures can rightfully be considered the first photo of your child. If the picture was successful, then you can see the profile of the baby, his pens, neck, tummy and head, legs and even the umbilical cord in the picture. Most of the questions arise on the recognition of sexual characteristics in such "photos". With boys, things are somewhat simpler, whereas the girl’s somewhat swollen external genitals is easy to take for a boy.
If the doctor assumes that you have a girl, ask him to take a “photo” in such a projection. If the location of the fruit will allow it to be done, then there will be less doubt.
- Twins. In the picture ultrasound twins, one baby is always better than the other. Infrequently, but it is possible that one baby hides behind another, and the doctor may mistakenly conclude that a woman carries only one fruit. Careful examination of the heartbeats should suggest that two hearts are beating. And the subsequent ultrasound examinations show grown twins or twins for sure.
You will learn about the ultrasound scan on the 12th week of pregnancy from the following video.